Clinical Trial Phases: What Each Stage Means for Drug Safety and Approval
When a new medicine hits the market, it didn’t just appear out of nowhere—it went through a strict series of tests called clinical trial phases, a structured process to evaluate the safety, dosage, and effectiveness of new drugs before they’re approved for public use. Also known as drug development stages, these phases are the backbone of how we know a medication is safe and works as intended. Without them, we’d be guessing whether pills actually help—or if they could hurt.
There are four main clinical trial phases, a step-by-step system used by regulators like the FDA to test new drugs in humans. Phase I, the first human test, focuses on safety and dosage—usually with 20 to 80 healthy volunteers. Researchers watch for side effects and figure out how the body handles the drug. Phase II, moves to patients with the target condition, often a few hundred people. Here, they check if the drug actually works for its intended purpose—like lowering blood pressure or reducing seizures—while still watching for side effects. Phase III, is the big one: thousands of patients across multiple locations, comparing the new drug to existing treatments or placebos. This is where regulators decide if the benefits outweigh the risks. And Phase IV, happens after approval, tracking long-term effects in the real world.
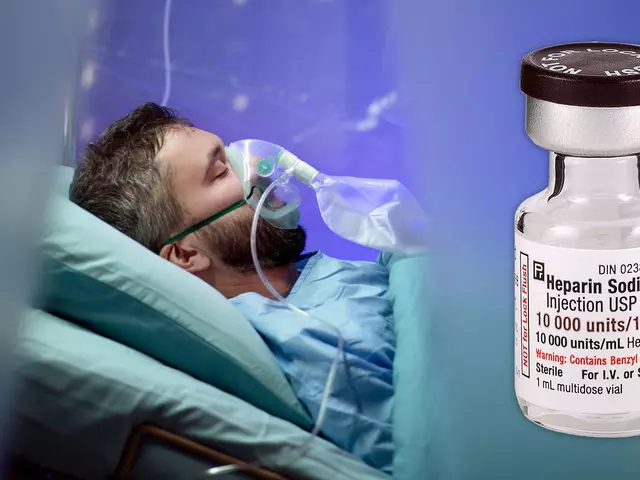
These phases aren’t just paperwork—they’re what keep you safe. That’s why you see so many posts here about generic drugs, FDA inspections, and bioequivalence studies. All of them tie back to what happens in these trials. For example, bioequivalence studies ensure generics work just like brand-name drugs, and that’s only possible because Phase III trials proved the original worked. Same with FDA inspections: they check if manufacturing sites can reliably produce what was tested in trials. Even genetic factors affecting drug reactions? That’s something researchers now look for during Phase I and II, especially in trials for antidepressants or pain meds.
What you’ll find in the posts below isn’t just random drug info—it’s all connected to how drugs get tested, approved, and monitored. From how age and sex affect trial design to why some people get diarrhea on vilazodone or why corticosteroids can trigger mood swings, every story here traces back to the clinical trial process. You’ll see how real-world results from these trials shape prescriptions, safety warnings, and even cost-saving strategies. This isn’t theory. It’s what’s in your medicine cabinet today.