Pre-Approval Inspection: What It Is and Why It Matters for Your Medications
When you pick up a new prescription, you trust that it’s safe, effective, and made the right way. That trust doesn’t come from luck—it comes from something called a Pre-Approval Inspection, a mandatory review and site visit by regulators before a new drug or generic version can be sold. Also known as a pre-approval inspection (PAI), it’s the final checkpoint before a medication reaches pharmacies and patients. This isn’t just paperwork. It’s a hands-on check of the factory, lab, and quality systems that make your pills, injections, or inhalers.
Think of it like a surprise audit for drugmakers. Regulators like the FDA don’t just read reports—they show up at manufacturing sites, walk through clean rooms, check equipment logs, and review how staff handle samples. They’re looking for one thing: consistency. If a batch of pills is made one way today and another way tomorrow, that’s a problem. Even small changes in temperature, mixing time, or raw material source can change how the drug works in your body. That’s why pharmaceutical quality, the system that ensures every dose is identical and meets strict standards is the backbone of every drug approval, the official process that lets a medication be legally sold. Without a clean Pre-Approval Inspection, even a perfectly designed drug can’t get to market.
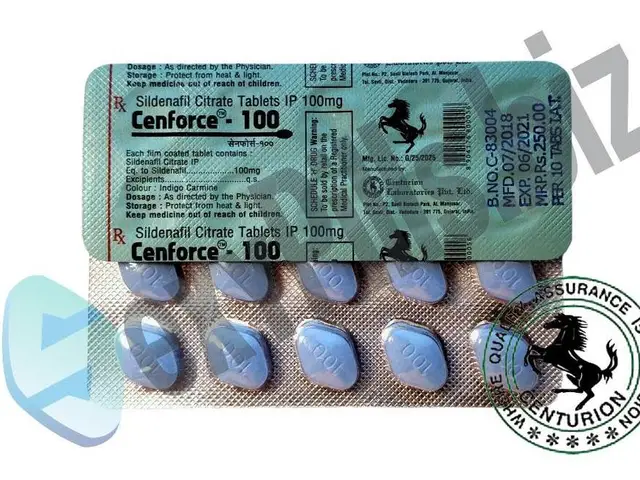
And it’s not just new drugs. Generic versions—like Tadalis SX or Cobix—are held to the same standard. If a company wants to sell a cheaper version of a brand-name medicine, they must prove their factory can make it just as well. That’s why FDA inspection, the official review process conducted by U.S. regulators to verify compliance is so critical. A single failed inspection can delay a drug for months—or kill it entirely. That’s why some medications never make it to shelves, even if the science works.
You might not see it, but Pre-Approval Inspection affects every pill you take. It’s why counterfeit drugs are rare in regulated markets. It’s why your blood pressure meds from last month work the same as this month. It’s why genetic reactions to drugs like vilazodone or ampicillin are studied in controlled environments before approval. This system protects you from bad batches, wrong dosages, and unsafe ingredients. And when something goes wrong—like a recall or a side effect spike—it’s often because this inspection missed something, or rules changed after the fact.
What you’ll find in the posts below are real-world examples of how drug safety, manufacturing, and regulation connect to your daily health. From how bioequivalence studies ensure generics work the same, to how patient vigilance helps spot fake pills, these stories show you what’s really going on before that bottle reaches your medicine cabinet. This isn’t just bureaucracy. It’s your safety net.