Understanding Abacavir and its Role in HIV Treatment
As a blogger passionate about health and well-being, I feel it is important to discuss the topic of Abacavir and liver health. Abacavir is a medication used in the treatment of HIV, specifically as part of antiretroviral therapy (ART). It helps in preventing the virus from multiplying, thus slowing down the progression of the disease. However, like any other medication, Abacavir has its fair share of side effects and potential health risks.
In this article, we will delve into the various aspects of Abacavir and its impact on liver health. The information provided here can be useful for those who are currently on Abacavir, considering starting it, or simply want to learn more about the medication and its effects on the body.
How Abacavir Works and its Importance in HIV Treatment
Before we dive into the effects of Abacavir on liver health, it is essential to understand how the medication works and why it is an important part of HIV treatment. Abacavir is a type of nucleoside reverse transcriptase inhibitor (NRTI). NRTIs work by blocking the action of an enzyme called reverse transcriptase, which HIV uses to replicate its genetic material. By blocking this enzyme, Abacavir effectively prevents the HIV virus from multiplying and spreading throughout the body.
Abacavir is often used in combination with other antiretroviral medications as part of ART. This approach helps in controlling the viral load, improving immune system function, and ultimately, delaying the progression of HIV into AIDS. With proper treatment and adherence to prescribed medications, people living with HIV can lead relatively healthy lives and have a near-normal life expectancy.
Potential Side Effects of Abacavir on Liver Health
While Abacavir is effective in managing HIV, it is not without its side effects. Some of these side effects can have an impact on liver health. Common liver-related side effects of Abacavir include an increase in liver enzymes, which can be an indication of liver inflammation or damage. In rare cases, Abacavir has been associated with liver failure, particularly in people with pre-existing liver disease or other risk factors for liver problems.
It is important to note that liver complications related to Abacavir use are relatively uncommon. The benefits of the medication in controlling HIV usually outweigh the risks associated with potential liver problems. However, it is crucial to monitor liver health while on Abacavir, particularly if you have pre-existing liver conditions or other risk factors.
Abacavir Hypersensitivity Reaction and its Relation to Liver Health
One of the most significant concerns regarding Abacavir use is the risk of a hypersensitivity reaction (HSR). This is an allergic reaction that can occur in some people who take the medication. Symptoms of Abacavir HSR may include fever, rash, gastrointestinal issues, respiratory problems, and in some cases, liver inflammation. If left untreated, Abacavir HSR can be life-threatening.
Fortunately, a genetic test called HLA-B*5701 screening is available to identify individuals who are at a higher risk of developing Abacavir HSR. If the test is positive, healthcare providers will recommend alternative antiretroviral medications to avoid the risk of HSR and potential liver complications.
Monitoring Liver Health While on Abacavir
Given the potential risks associated with Abacavir and liver health, it is important to have regular liver function tests while on the medication. These tests help in monitoring liver enzyme levels, which can indicate possible liver inflammation or damage. If any abnormalities are detected, healthcare providers can adjust the treatment plan accordingly to minimize the risk of liver complications.
It is also essential to discuss any pre-existing liver conditions or risk factors with your healthcare provider before starting Abacavir. In some cases, alternative medications may be recommended to reduce the risk of liver complications.
Managing Liver Health While on Abacavir
While taking Abacavir, there are several lifestyle choices and habits that can help maintain liver health and minimize the risk of complications. These include:
- Avoiding excessive alcohol consumption, as it can exacerbate liver damage.
- Maintaining a balanced diet, rich in fruits, vegetables, and whole grains to support liver function.
- Exercising regularly to help maintain a healthy weight and reduce the risk of fatty liver disease.
- Taking prescribed medications as directed and discussing any potential interactions with your healthcare provider.
- Regularly monitoring liver function and promptly addressing any abnormalities with your healthcare provider.
By being proactive about liver health, individuals taking Abacavir can minimize the risk of liver complications and maintain a better overall quality of life.










The article grossly oversimplifies the hepatic ramifications of abacavir, ignoring the nuanced pharmacodynamics that seasoned clinicians appreciate. Moreover, it fails to address the interplay between antiretroviral regimens and co‑morbid liver conditions, which is a critical oversight. Such a shallow treatment of the subject does a disservice to patients seeking comprehensive guidance. The tone is alarmist yet devoid of the rigorous evidence required for sound medical advice.
I understand the frustration, but let’s remember that many patients on abacavir do fine with routine monitoring 😊. The key is consistent liver function testing and open dialogue with your provider. Even if the article feels alarmist, it does raise awareness, which can be beneficial when paired with professional counsel.
Honestly, this piece reads like a watered‑down brochure written for the medically ill‑informed. It certainly pretends to be exhaustive, yet it skims over the seminal trials that actually define abacavir’s safety profile. One would expect a deeper dive into hepatic enzyme dynamics, but instead we get generic lifestyle tips. Defintely not the kind of analysis a serious clinician craves.
It’s helpful to see a balanced overview that acknowledges both the benefits and the risks of abacavir, especially for those dealing with liver concerns. While the article could expand on the mechanisms, it does a decent job of reminding readers about regular monitoring and lifestyle factors.
From a pharmacokinetic standpoint, abacavir’s nucleoside analogue activity necessitates vigilant hepatic surveillance, particularly in poly‑therapy contexts where cytochrome‑P450 interactions may modulate enzyme levels. The author’s emphasis on integrated care pathways aligns with current therapeutic guidelines, though the omission of specific ALT/AST threshold values is notable.
We must not trivialize the moral responsibility of prescribing physicians; ignoring potential hepatotoxicity is tantamount to negligence. Even if the article is well‑intentioned, it skirts around the ethical obligation to fully inform patients about rare but severe outcomes.
Oh sure, the “clinical trial data” is all sunshine and rainbows, but did anyone mention the hidden agenda of pharmaceutical giants pushing abacavir as the silver bullet? Let’s not forget that every “increase in liver enzymes” could be a silent alarm, a covert signal that the government wants us to ignore. The whole narrative feels like a staged propaganda piece, designed to keep us complacent while the elite profit.
Monitoring liver enzymes regularly is crucial.
It’s infuriating how these health articles always sidestep the true patriot’s duty to protect our nation’s wellbeing! We should demand that our leaders prioritize locally sourced medications that respect our sovereignty, not foreign compounds that might jeopardize our liver health.
Hey folks, just wanted to say that staying on top of your liver tests while on abacavir can actually be empowering. Small steps like avoiding excess booze and eating greens go a long way, and you’ll feel better for it.
According to the latest peer‑reviewed literature, the incidence of clinically significant hepatotoxicity in patients adhering to abacavir‑based regimens is approximately 0.5 % per annum. This figure is derived from pooled data across multiple Phase III trials, with rigorous statistical adjustments for confounding variables. Hence, the risk, while present, remains low when proper monitoring protocols are followed.
Let’s keep the conversation respectful and focus on actionable steps. If you notice any unusual symptoms, schedule a check‑up right away-early detection can prevent serious complications. Remember, your liver is resilient, but it needs your support.
Honestly, I think the whole emphasis on liver monitoring is overblown; most patients never experience severe issues, so why the hype? It feels like they’re trying to sell anxiety instead of useful information.
🚀 Let’s rally together and make liver health a community priority! Share your success stories, swap healthy recipes, and encourage each other to stay on top of those labs. We’ve got this, team! 🌟
As a proud citizen, I must stress that we cannot blindly trust foreign pharma narratives that downplay hepatic risks. It is our duty to demand transparent, homegrown solutions that safeguard our people’s livers without compromising national pride.
Abacavir remains a cornerstone of modern antiretroviral therapy, offering potent viral suppression for millions worldwide.
Nevertheless, its interaction with hepatic pathways warrants vigilant observation, especially in cohorts with pre‑existing liver disease.
Routine measurement of ALT and AST levels every three to six months provides an early warning system that can avert catastrophic outcomes.
If elevations exceed three times the upper limit of normal, clinicians should consider dosage adjustment or switching to an alternative NRTI.
Patients should be educated to recognize subtle symptoms such as unexplained fatigue, jaundice, or abdominal discomfort, which may herald hepatic distress.
Lifestyle modifications play an equally pivotal role; limiting alcohol intake reduces oxidative stress on hepatocytes.
A diet rich in antioxidants-think berries, leafy greens, and omega‑3 fatty acids-can bolster hepatic resilience.
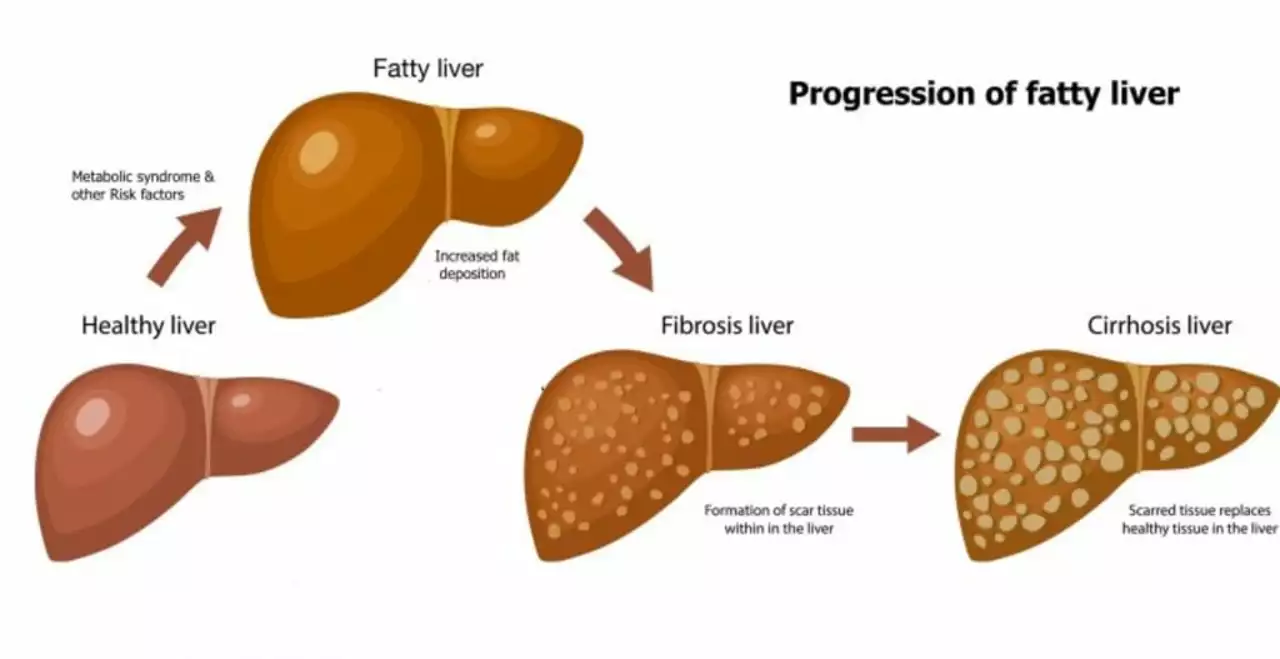
Regular physical activity improves insulin sensitivity, thereby decreasing the risk of non‑alcoholic fatty liver disease, a common comorbidity in HIV‑positive individuals.
Moreover, clinicians must review concomitant medications for potential hepatotoxic interactions, as polypharmacy is a frequent reality in this population.
Pharmacogenomic testing, such as HLA‑B*5701 screening, not only predicts hypersensitivity reactions but also informs personalized liver safety strategies.
Open communication between patient and provider fosters adherence to monitoring schedules and encourages prompt reporting of adverse events.
In resource‑limited settings, point‑of‑care liver function tests can bridge gaps in laboratory access, ensuring timely intervention.
Community support groups offer psychosocial reinforcement, reminding patients that liver health is a shared responsibility.
Ultimately, a proactive, multidisciplinary approach transforms the abstract risk of hepatotoxicity into a manageable component of comprehensive HIV care.
By integrating vigilant monitoring, lifestyle stewardship, and collaborative care, we empower patients to thrive while safely navigating the complexities of abacavir therapy.