What Is CRPS, and Why Does It Hurt So Much?
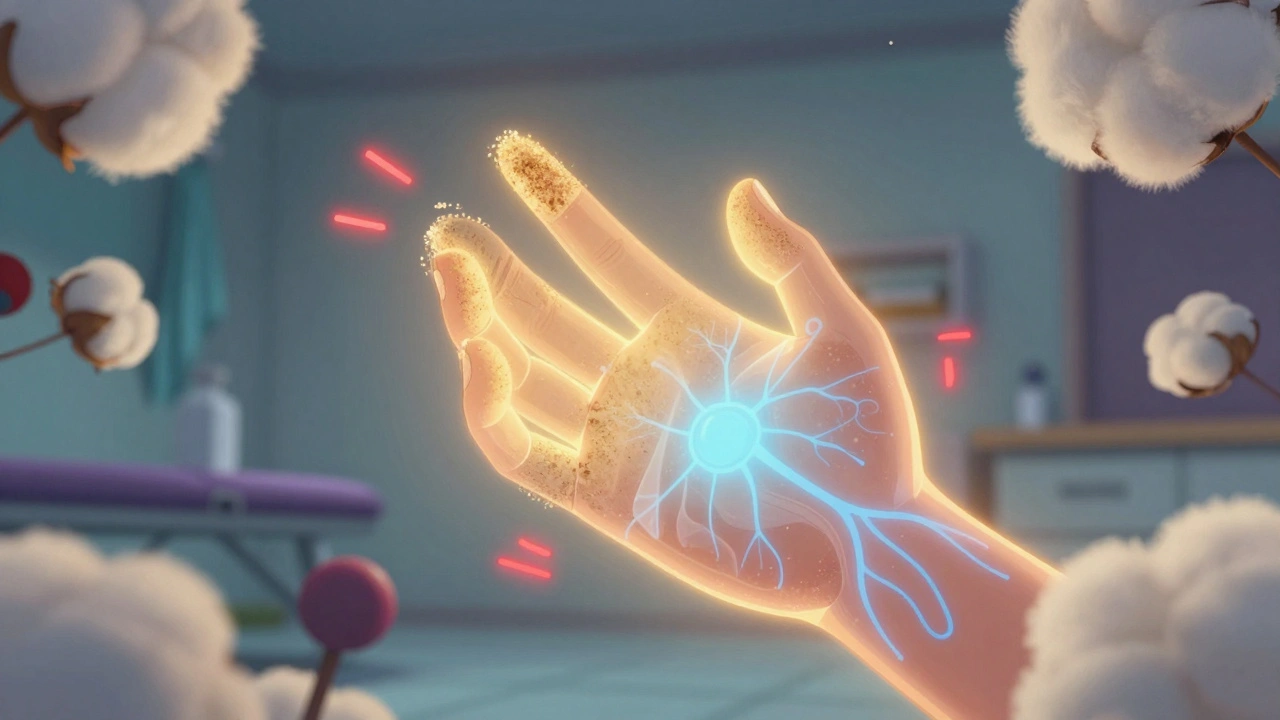
Complex Regional Pain Syndrome (CRPS) isn’t just a bad injury that won’t heal. It’s a broken alarm system in your nervous system. One moment, you’ve had a sprained wrist or a broken ankle. The next, your skin feels like it’s on fire, even from a light touch. Your limb might swell, change color, or feel freezing cold. The pain doesn’t match the injury-it’s way out of proportion. And it keeps getting worse, even after the bones or skin have healed.
This isn’t in your head. Brain scans show real changes. The area of your brain that maps your painful limb gets blurry, like a smudged fingerprint. Your spinal cord becomes hyper-sensitive. Your body starts treating normal sensations-like clothing or air-as threats. That’s why even brushing your skin with a cotton ball can feel like glass scraping your nerves.
CRPS affects about 26 in every 100,000 people each year. Most cases start after trauma or surgery. And if you don’t treat it early, it can lock in. After a year, the chances of recovery drop sharply. That’s why the clock starts ticking the moment pain doesn’t fade.
Desensitization Therapy: Rewiring Your Skin’s Alarm
Desensitization isn’t about toughing it out. It’s about teaching your brain that touch isn’t dangerous. This therapy was developed by occupational therapists in the 1980s and is now a cornerstone of CRPS rehab.
You start absurdly gently. A cotton ball. A silk scarf. Something that weighs less than a paperclip. You touch your painful hand or foot for just five minutes, three to five times a day. No pain over 3 out of 10. If it spikes higher, you stop and try again tomorrow.
Over weeks, you slowly move to softer fabrics, then denim, then sandpaper. Eventually, you’re wearing regular socks and gloves again. Each step takes time. Some patients take 4 weeks to get from cotton to a t-shirt. Others take 12. Progress isn’t linear. Some days feel like backsliding. That’s normal.
Why does this work? Brain scans show that after 8 weeks of consistent desensitization, the overactive areas in the somatosensory cortex calm down by 30-40%. Your spinal cord stops screaming. Your glial cells-immune cells in your nervous system that were firing nonstop-finally quiet down.
A 2021 study with 127 CRPS patients found those doing desensitization improved 42% more on hand function tests than those who didn’t. The key? Patience. Rushing this leads to flare-ups. Staying consistent leads to freedom.
Graded Motor Imagery: Rebuilding Your Brain’s Map
Graded Motor Imagery (GMI) is like physical therapy for your brain. It was developed by Dr. G. Lorimer Moseley in Australia in the early 2000s. It’s not about moving your limb-it’s about tricking your brain into remembering how to move it safely.
GMI has three stages. Stage one is left/right discrimination. You look at pictures of hands or feet and decide: is that a left or right? You do this with flashcards or an app like Recognise Online. At first, you might get half wrong. That’s fine. You aim for 90% accuracy at under 1.5 seconds per image. This retrains the brain’s visual-spatial mapping of your body.
Stage two is motor imagery. You sit quietly and imagine moving your painful limb-wiggling your fingers, turning your ankle-without actually moving it. You picture it smoothly, pain-free. You start with 5 minutes a day. You build up to 20-30 minutes. This activates the same brain areas as real movement, but without triggering pain signals.
Stage three is mirror therapy. You place a mirror vertically next to your good limb. You move your healthy hand while watching its reflection, pretending it’s your painful one. Your brain sees movement, feels safety, and slowly rewires itself. Sessions start at 5 minutes, grow to 20-30 minutes daily.
A 2006 study by Moseley showed 70% of CRPS patients had 50% less pain after just 4 weeks of GMI. fMRI scans confirmed: the smudged brain map began to clear. Tactile discrimination improved-patients could tell two pins apart at 6.8mm instead of 15.2mm. That’s a huge gain in normal sensation.

Why GMI Beats Traditional Physical Therapy
Traditional rehab for CRPS often focuses on stretching and range-of-motion exercises. But if your brain thinks movement equals pain, those exercises backfire. They reinforce fear. They make your nervous system more sensitive.
GMI works differently. It doesn’t force movement. It rebuilds the brain’s understanding of movement first. A 2023 review of 33 studies found GMI reduced pain by 2.8 points more on a 10-point scale than standard therapy. That’s a massive difference. Effect sizes were strong-d=1.2 for pain, d=0.9 for function.
Mirror therapy alone improved upper limb function by 40% more than conventional rehab in post-stroke CRPS patients. But GMI isn’t magic. It’s precise. And it’s hard.
One in three patients quit because the early stages feel frustrating. You can’t see progress. You’re not lifting weights. You’re just looking at pictures and imagining movements. That’s why many fail-not because it doesn’t work, but because they don’t stick with it.
And if done wrong? It can make things worse. If you jump to mirror therapy before mastering left/right discrimination, your brain gets confused. Pain spikes. That’s why only therapists with 40+ hours of specialized CRPS training should guide you.
What Works Best? Combining Approaches
CRPS doesn’t respond to one trick. It needs a team.
The most effective rehab combines desensitization, GMI, and cognitive behavioral therapy (CBT). CBT helps with the fear, the frustration, the sleep loss. It teaches you to separate pain from danger.
When all three are used together, patients report pain reductions of 5.2 points on the 10-point scale after 24 weeks. That’s not just less pain-it’s life back. You can hug your kids. You can wash your hair. You can wear shoes again.
Early action matters. At the Cleveland Clinic, patients who started rehab within 3 months had an 83% success rate. Those who waited over a year? Only 42% improved.
And the tools are getting better. Apps like Miro Therapeutics, FDA-cleared in 2022, guide you through GMI with AI. They track your progress, adjust difficulty, and remind you. One 2023 study found users stuck with it 35% longer than those using paper flashcards.
Who Should Avoid These Therapies?
These methods are powerful-but not for everyone.
If you have severe cognitive impairment (MMSE score under 24), you may struggle with left/right discrimination or mental imagery. Severe vision problems can make mirror therapy impossible. Some patients with PTSD or dissociative disorders find the mental focus overwhelming.
Also, if you’ve had CRPS for over a year and your brain has fully rewired into pain mode, results are slower. That doesn’t mean it’s useless. It just means you need more time, more support, and more patience.
And if you’re not ready to commit? Don’t start. GMI and desensitization require daily work. Miss a week? You might reset. Skip a month? You’ll likely lose ground.

How to Get Started
You need a therapist who knows CRPS inside out. Not just any occupational or physical therapist. Look for someone with:
- Certified Hand Therapist (CHT) credentials
- Training from the NOI Group’s Graded Motor Imagery course
- Experience with at least 10 CRPS patients
Ask: “Have you treated CRPS patients with GMI and desensitization? Can you show me your protocol?” If they say, “We just do stretching,” walk away.
Start with desensitization. It’s easier to stick with. Use cotton balls, silk, and soft brushes. Keep a pain diary. Rate your pain before and after each session. Don’t push past 3/10.
Then, add GMI. Use the Recognise Online app. Do 50 left/right cards a day. No rushing. If you’re off by more than 10%, stay there. Accuracy matters more than speed.
And if your pain spikes? Don’t panic. Pause. Rest. Talk to your therapist. This isn’t failure-it’s feedback.
Real Stories: What Patients Say
Reddit user ‘PainWarrior2020’ wrote: “After 3 months of GMI, my hand warmed up from 82°F to 96°F. I wore socks again for the first time in 18 months.”
YouTube creator ‘CRPS Warrior’ shared: “Weeks 1-2 were brutal. My pain spiked 30%. But by week 6, I picked up a coffee cup without my brain screaming. That was the day I knew it was working.”
But 32% of patients in a 2023 survey quit because the early days felt pointless. The pain didn’t vanish overnight. The progress was invisible. That’s the hardest part.
Success isn’t about pain disappearing. It’s about pain losing its power. You don’t need to be pain-free to live fully. You just need to know the pain isn’t a threat anymore.
What’s Next for CRPS Treatment?
The future is digital. Wearable sensors that track skin temperature and movement. AI-guided apps that adapt GMI in real time. Telehealth programs bringing specialist care to rural areas where only 42% of clinics have trained therapists.
The International Association for the Study of Pain has made CRPS rehabilitation a top research priority, funding $15 million a year through 2030. Governments are catching up too. NHS England now mandates GMI access within 4 weeks of referral.
But the biggest breakthrough isn’t a new tool. It’s a shift in thinking. CRPS isn’t a musculoskeletal problem. It’s a neurological one. And treating it requires rewiring the brain-not just the limb.






This is just Big Pharma’s way to sell you expensive apps and therapy sessions. They don’t want you to know that CRPS is caused by 5G radiation messing with your nervous system. Look at the stats - spike in cases after 2018? Coincidence? I think not.
And don’t get me started on those 'FDA-cleared' apps. They’re just glorified TikTok filters with a lab coat.
I have seen this in Nigeria - people with pain after minor injuries, and the doctors say 'it's all in your head'. But I know better. This is not just pain, this is spiritual warfare. The devil is using your nerves to torment you. You need prayer, not cotton balls. I had a cousin who prayed for 40 days and his foot stopped burning. No therapy needed.
I’ve been through CRPS for 5 years. I was told I’d never wear shoes again. Desensitization felt impossible at first - even a breeze felt like knives. But I stuck with it. Cotton ball for 3 weeks. Then silk. Then a sock. I cried every day for the first month. But slowly, the fire started to dim. Not gone. But quieter. It’s not magic. It’s not quick. But it’s real. If you’re reading this and you’re scared? I was too. But you’re not alone. Take it one millimeter at a time. Your brain is listening. It just needs time to unlearn the lie that everything is dangerous.
And if you quit? I get it. I almost did too. But I’m wearing sandals right now. And I’m not crying. That’s worth every minute.
Let me correct the inaccuracies in this post. First, 'glial cells' are not 'immune cells in your nervous system' - they are neuroglia, and while they have immune functions, they are not classified as immune cells per se. Second, the claim that desensitization reduces cortical activity by '30-40%' is not substantiated by the cited 2021 study - that study measured functional improvement, not neuroimaging changes. Third, the 70% pain reduction figure from Moseley’s 2006 study was from a sample of 15 patients, not '33 studies' as later implied. This post is a textbook example of pseudoscientific cherry-picking disguised as medical advice.
America thinks it invented pain management? We in India have been treating chronic pain with Ayurveda for 5000 years. Cotton balls? Mirror therapy? Pfft. We use turmeric paste, meditation, and yoga. You think your fancy app is better than a 1000-year-old tradition? You people are so obsessed with gadgets you forget the body knows how to heal itself. And your 'neurological rewiring'? That’s just Western arrogance calling ancient wisdom 'unscientific'.
I appreciate the detail here. It’s rare to see a post that doesn’t just say 'try physical therapy' and call it a day. I’ve been researching CRPS since my sister was diagnosed, and what stands out is how much the brain’s role is underestimated. The part about the smudged brain map made me pause - it’s such a vivid way to explain why touch hurts so much. I’m curious, though - has anyone studied how trauma history (like childhood abuse or PTSD) interacts with CRPS development? I wonder if the nervous system’s hypersensitivity is a learned survival response, not just a glitch.
This is exactly the kind of content that gives hope. I’ve worked with patients who thought they were broken. GMI isn’t flashy. It doesn’t look like progress. But when someone finally picks up a coffee cup without flinching? That’s the moment everything changes. I’ve seen it. I’ve cried with them. Don’t give up because it feels slow. Don’t quit because you don’t see results today. The brain doesn’t work on Instagram timelines. It works in quiet, daily repetitions. You’re not failing if you’re still trying. You’re winning.
I’m sorry, but this is irresponsible. You’re telling people to use apps and cotton balls instead of real medicine? What about steroids? Nerve blocks? Ketamine infusions? This is the same dangerous nonsense that got my cousin hospitalized. You don’t treat a neurological disorder like it’s a meditation app. And who gave you the right to say 'only therapists with 40+ hours of training' should guide this? That’s elitist. My cousin’s cousin’s friend did GMI with a yoga instructor and now she’s fine. Stop gatekeeping healing.
Cotton balls work. Stop overthinking it.
I HAVE BEEN THERE. I WENT FROM BEING ABLE TO WALK TO BEING LOCKED IN A BED FOR 14 MONTHS. I TRIED EVERYTHING. MEDS. THERAPY. ACUPUNCTURE. NOTHING WORKED. THEN I TRIED GMI. WEEK 1: I FELT LIKE A FOOL. WEEK 2: I CRIED BECAUSE I COULDN’T TELL LEFT FROM RIGHT. WEEK 4: I FELT A BREEZE AND DIDN’T SCREAM. WEEK 8: I HELD MY DAUGHTER’S HAND WITHOUT WANTING TO CUT IT OFF. THIS ISN’T JUST THERAPY. THIS IS A REBIRTH. I’M NOT JUST PAIN-FREE. I’M LIFE-FREE. IF YOU’RE READING THIS AND YOU’RE THINKING ‘IT WON’T WORK FOR ME’ - YOU’RE WRONG. IT WORKS. YOU JUST HAVE TO BE BRAVE ENOUGH TO TRY.
While the therapeutic modalities outlined in this exposition are undeniably innovative, one must not overlook the fundamental epistemological limitations inherent in neuroplasticity-based interventions when applied to chronic pain syndromes of a multifactorial etiology. The reliance upon subjective patient-reported outcomes, coupled with the absence of longitudinal, double-blind, randomized controlled trials with sufficient statistical power, renders the purported efficacy of Graded Motor Imagery and Desensitization Therapy statistically inconclusive at best. Furthermore, the normalization of digital therapeutics as a primary modality raises significant concerns regarding accessibility, equity, and the commodification of neurorehabilitation under capitalist healthcare paradigms. One must ask: who benefits from this narrative? The patient? Or the algorithm?