
Understanding Heparin Sodium and its Role in Anticoagulation Therapy
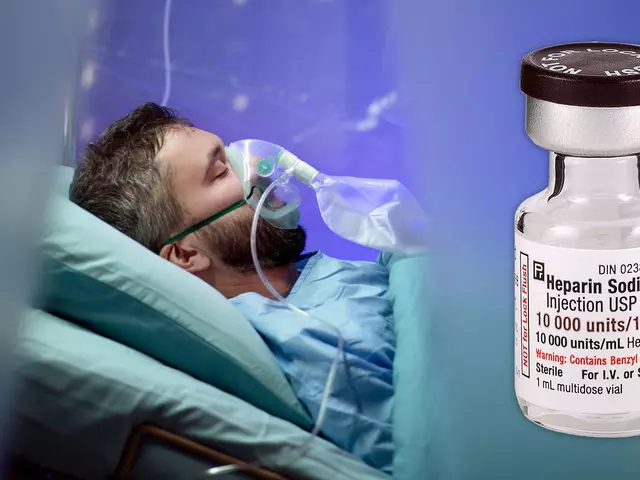
Before we delve into the relationship between heparin sodium and exercise, let's first understand what heparin sodium is and its role in anticoagulation therapy. Heparin sodium is a medication that is often prescribed to prevent blood clots from forming or growing. This is vital in cases such as deep vein thrombosis or pulmonary embolism. As a part of anticoagulation therapy, heparin sodium ensures that our blood does not coagulate or clot excessively, which could lead to severe health complications. So, if you're on this therapy, it means you need to take extra care in your daily activities, including exercise.
The Importance of Exercise in Anticoagulation Therapy
Now, you might be wondering how exercise fits into all of this. Well, regular physical activity is essential for maintaining good health, and this is no different for those undergoing anticoagulation therapy. Exercise helps boost circulation, strengthen the heart, and improve overall cardiovascular health. However, it's crucial to approach exercise with caution and awareness, as certain activities can potentially increase the risk of bleeding or bruising while on anticoagulation therapy.
Choosing Appropriate Exercises
When choosing exercises, it's vital to consider those that are less likely to cause injury. The risk of falling or getting bruised can be higher when you're on anticoagulation therapy. Therefore, exercises like walking, cycling, swimming, or doing yoga are great options. These activities are low impact and less likely to lead to injuries, yet they provide excellent cardiovascular benefits.
Understanding the Risks
While exercise is beneficial, it's also important to understand the potential risks. When on heparin sodium, your blood's ability to clot is reduced. This means that if you get injured, you could bleed more than someone who is not on this medication. Thus, activities that carry a high risk of falls or injuries, like contact sports or mountain climbing, should be avoided.
Consulting with Your Healthcare Provider
Before starting any new exercise routine, it's imperative to consult with your healthcare provider. They know your medical history, current health status and can provide personalized advice. They can guide you on what exercises are safe for you to do and what precautions you need to take.
Monitoring Your Body's Response
It's important to listen to your body and monitor your response to exercise. If you feel dizzy, lightheaded, or experience unusual shortness of breath, it's crucial to stop exercising immediately and seek medical attention. These could be signs that your body isn't responding well to the physical activity.
Maintaining Hydration and Nutrition
Hydration and nutrition are key elements in any exercise routine, especially if you're on anticoagulation therapy. Staying hydrated helps prevent blood from becoming too thick, which can increase the risk of clotting. Similarly, eating a well-balanced diet can help maintain your energy levels and overall health while on therapy.
Importance of Regular Check-ups
Regular check-ups are essential when you're on anticoagulation therapy. Your healthcare provider may need to adjust your medication dosage based on your body's response to the treatment. Regular blood tests can help monitor the effectiveness of your treatment and ensure that your blood is not too thin, which can increase the risk of bleeding.
Living a Balanced Lifestyle
Living a balanced lifestyle is crucial when on anticoagulation therapy. This means eating a healthy diet, getting regular exercise, and taking time to rest and relax. It's all about creating a balance that allows you to stay active and healthy while managing your treatment effectively.
Staying Positive and Motivated
Last but not least, maintaining a positive attitude and staying motivated is key. Being on anticoagulation therapy can be challenging, but it's important to remember that it's for your well-being. Exercise can be a great way to boost your mood and keep you motivated. Remember, every step you take is a step towards a healthier you.






Living with heparin sodium can feel like walking a tightrope between safety and activity.
Yet the very purpose of anticoagulation is to keep our vessels clear, which in turn grants us the freedom to move.
If we allow fear of bleeding to imprison us, we defeat the therapy’s ultimate goal.
Exercise, when chosen wisely, becomes a gentle force that circulates blood and strengthens the heart without demanding undue risk.
Low‑impact pursuits such as walking, swimming, or yoga serve as the perfect companions to a regimen of heparin, offering cardiovascular benefits while keeping the chance of trauma minimal.
Moreover, the rhythm of regular movement supports the endothelial lining, which can subtly enhance the body’s own antithrombotic mechanisms.
It is crucial, however, to stay vigilant; any unexpected bruising or prolonged bleeding should prompt an immediate check‑in with a clinician.
Hydration, as the article notes, keeps the blood from becoming overly viscous, and a well‑balanced diet supplies the nutrients necessary for tissue repair.
In this delicate dance, the guidance of a healthcare provider functions as the choreographer, ensuring each step is measured and safe.
When planning a new routine, start with short sessions, monitor how your body feels, and gradually increase intensity.
Pay attention to signs such as dizziness, excessive fatigue, or unusual shortness of breath, as they may indicate that the current load is too demanding.
The psychological boost derived from consistent activity also cannot be overstated; a positive mindset fuels adherence to medication and lifestyle changes alike.
Collaborative support from friends, family, or online communities provides accountability and shared wisdom, making the journey less solitary.
Ultimately, the partnership between heparin therapy and thoughtful exercise is not a contradiction but a harmonious alliance that promotes longevity and quality of life.
Embrace the possibility of movement, respect the limits of your body, and you will discover that even under anticoagulation, a vibrant, active life is within reach.
Great advice! A brisk walk each morning or a gentle yoga session can boost circulation while keeping risk low.
Keep it consistent and stay hydrated!
Your concerns about bruising are understandable, and it’s wise to choose activities that minimize impact.
Walking, cycling, and swimming all provide solid cardio without demanding harsh contact.
Listening to your body’s signals will guide you toward the right intensity.
Remember, modest progress each week adds up to significant health benefits over time.
The proposition that all forms of exercise are uniformly beneficial under heparin therapy is a simplistic fallacy.
While low‑impact modalities are indeed commendable, one must eschew any semblance of reckless exuberance that could precipitate hemorrhagic complications.
It is incumbent upon the patient to solicit precise directives from a qualified clinician before embarking upon any regimen.
Moreover, the dietary counsel regarding hydration and nutrition should be adhered to with scrupulous exactitude, lest inadvertent hypercoagulability arise.
In sum, disciplined prudence outweighs cavalier enthusiasm.
One could argue that the article merely regurgitates common sense, cloaking it in medical jargon.
Nevertheless, such platitudes serve as a veneer for complacency.
Exercise on heparin? Fine.
It is morally reprehensible to ignore the obvious hazards of high‑impact sports while on anticoagulants.
One must act with prudence.
Discipline is the cornerstone of safe living.
Let us not be divided by fear; instead, we should embrace responsible activity with confidence and compassion.
By asserting our right to move, we honor both our bodies and the medical guidance we receive.
Together we can create a supportive environment where safe exercise thrives.
It is our duty to champion this balanced approach.
From a cardiometabolic perspective, incorporating low‑impact aerobic modalities-such as steady‑state cycling or pool‑based interval training-optimizes shear stress and endothelial function without elevating hemorrhagic risk.
Pair this with periodized strength conditioning to maintain musculoskeletal integrity, and you achieve a comprehensive, evidence‑based protocol.
Consistent monitoring of INR levels will ensure therapeutic windows remain intact.