
LASIK Inflammation Risk Calculator
Risk Assessment Tool
Answer these questions to determine your personalized inflammation risk level after LASIK surgery.
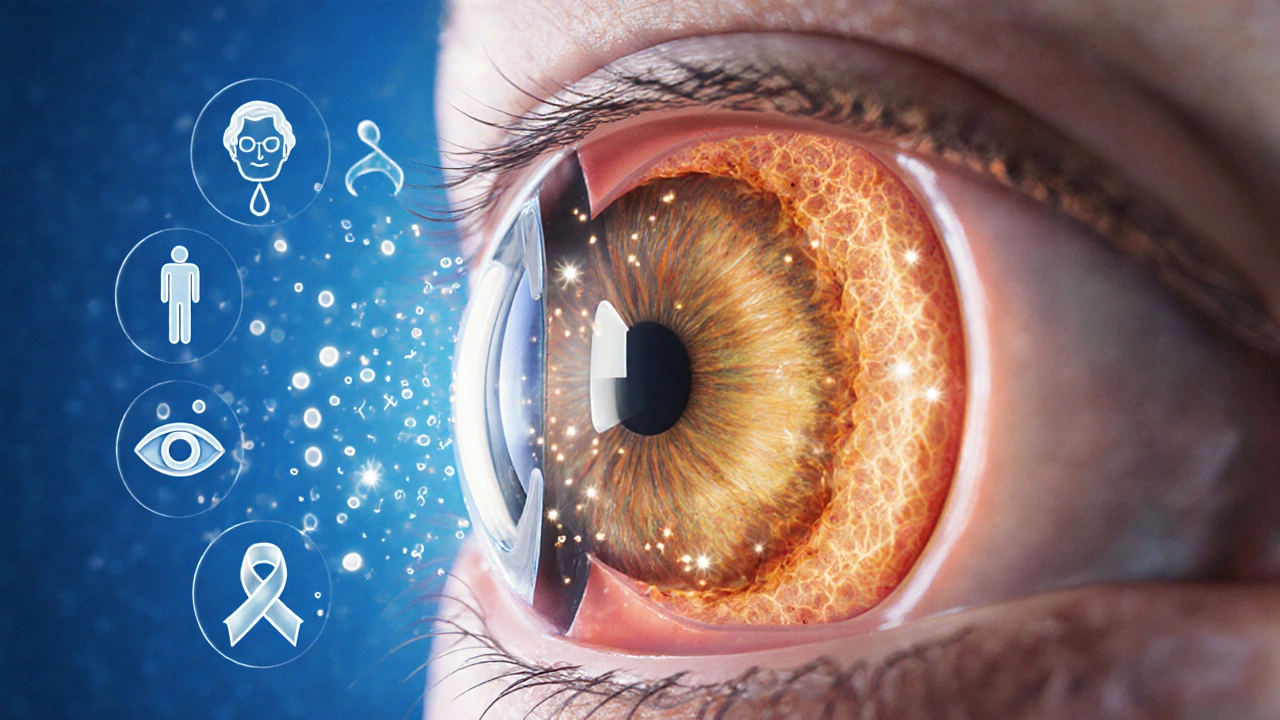
When a patient undergoes LASIK surgery, a laser reshapes the cornea to correct nearsightedness, farsightedness, or astigmatism. After the corneal flap is created, postoperative inflammation is the body’s natural healing response. While some swelling is expected, excess inflammation can sabotage the visual gains that LASIK promises.
- Even mild inflammation can blur vision for days to weeks.
- Severe inflammation raises the risk of haze, regression, and dry‑eye symptoms.
- Early detection and proper medication dramatically improve final visual acuity.
- Patient‑specific factors like age and pre‑existing dry eye influence inflammation severity.
- Follow‑up protocols that track corneal thickness and inflammation markers cut complication rates in half.
What is postoperative inflammation in the LASIK eye?
The cornea’s outer layer, the corneal epithelium, is gently lifted to create a flap. This mechanical disruption triggers the release of cytokines, prostaglandins, and other inflammatory mediators. The result is a temporary swelling of the stromal tissue and an influx of white blood cells. In most cases the swelling peaks within 24‑48hours and resolves without lasting impact, but when the cascade runs unchecked, it can lead to stromal haze or even flap‑edge inflammation.
How inflammation translates into visual outcomes
The primary goal of LASIK is to achieve a sharp, stable visual acuity. Inflammation interferes in three main ways:
- Optical distortion - Swollen stromal fibers change the cornea’s curvature, causing ghosting or fluctuating vision.
- Delayed epithelial healing - When the epithelium re‑grows slowly, patients may experience glare, halos, and reduced contrast sensitivity.
- Regression - Persistent inflammatory signaling can remodel the cornea back toward its pre‑surgery shape, eroding the refractive correction.
Studies published in the Journal of Refractive Surgery (2023) reported that eyes with high‑grade inflammation at day3 were three times more likely to need a touch‑up procedure within six months.
Risk factors that amplify the inflammatory response
Not everyone reacts the same way. The following variables tip the balance toward excessive swelling:
- Age - Older patients have slower cellular turnover, prolonging the inflammatory phase.
- Pre‑existing dry eye - Measured by reduced tear break‑up time (<10seconds), dry eye predisposes the cornea to inflammation.
- Auto‑immune conditions such as rheumatoid arthritis or lupus increase systemic cytokine levels.
- Medications - Certain antihistamines and isotretinoin can impair healing.
- Flap creation technique - Microkeratome flaps tend to produce more mechanical stress than femtosecond lasers.
Managing inflammation: the pharmacological toolkit
The standard of care involves a combination of topical corticosteroid drops and, when needed, non‑steroidal anti‑inflammatory drugs (NSAIDs). Here’s how they work:
| Medication | Mechanism | Typical Duration | Key Considerations |
|---|---|---|---|
| Prednisolone acetate 1% | Inhibits cytokine production | 1‑4weeks (tapered) | Monitor intra‑ocular pressure |
| Loteprednol etabonate 0.5% | Soft‑steroid, less IOP rise | 2‑3weeks | Preferred for glaucoma risk |
| Ketorolac 0.5% | Blocks prostaglandin synthesis | 5‑7days | Avoid in patients with corneal ulcers |
Patients with severe inflammation may also benefit from a short course of oral steroids, but this approach is reserved for cases where topical therapy fails to curb swelling within the first 48hours.
Monitoring and follow‑up: catching problems early
Because the window for intervention is narrow, surgeons schedule visits on day1, day3, week1, and month1 post‑op. The following metrics are routinely recorded:
- Uncorrected distance visual acuity (UDVA)
- Corneal pachymetry - a rise of >10µm signals lingering edema.
- Anterior segment OCT - visualizes micro‑haze or flap interface inflammation.
- Tear film assessment - informs adjunct dry‑eye therapy.
The postoperative inflammation that follows LASIK can be mitigated when clinicians act on these data points promptly.
Real‑world case snapshots
CaseA: A 28‑year‑old myope with no dry‑eye history reported blurry vision on day2. Pachymetry showed a 12µm increase. The surgeon intensified prednisolone to four times daily; by day5, UDVA improved from 20/40 to 20/20.
CaseB: A 52‑year‑old hyperope on antihistamines developed persistent haze at week2. NSAID therapy alone was insufficient; a switch to loteprednol with a slow taper resolved the haze over four weeks, avoiding a secondary PRK.

Pre‑surgery steps to limit inflammation
Patients can take proactive measures:
- Complete a dry‑eye work‑up and start preservative‑free lubricants at least two weeks before surgery.
- Discontinue isotretinoin and high‑dose omega‑3 supplements at least one month prior.
- Schedule the procedure when the immune system is not under stress (no recent infections or vaccinations within 48hours).
- Discuss any autoimmune conditions with the surgeon so prophylactic steroids can be planned.
These steps reduce the baseline inflammatory load, giving the cornea a smoother recovery.
Bottom line
While LASIK’s safety record remains excellent, the small fraction of patients who experience heightened postoperative inflammation can see a noticeable dip in visual quality. By recognizing risk factors, applying the right medication regimen, and adhering to a strict follow‑up schedule, clinicians can keep inflammation in check and preserve the crisp, stable vision patients expect.
Frequently Asked Questions
How long does normal inflammation last after LASIK?
Typical swelling peaks within 24‑48hours and resolves by day7 to 10 for most patients. Persistent symptoms beyond two weeks merit a re‑examination.
Can I use over‑the‑counter anti‑inflammatories after LASIK?
Oral NSAIDs are generally avoided because they can impair corneal healing. Stick to the surgeon‑prescribed drops and ask before adding any OTC medication.
What signs indicate severe inflammation?
Redness that spreads beyond the flap edge, increasing pain, a rise in corneal thickness >10µm, and a sudden drop in uncorrected visual acuity are red flags.
Do steroids increase the risk of infection?
When used as directed, the risk is low. However, patients must avoid contaminating the dropper and report any new discharge immediately.
Is there a link between dry eye and inflammation?
Dry eye reduces tear film stability, which can exacerbate inflammatory cytokine release. Treating dry eye before and after surgery helps keep inflammation in check.






Wow, the post really dives deep into the post‑surgery inflammation thing. I’ve actually seen a couple of friends go through LASIK and they told me that keeping the eye clean is key. Also, staying away from spicy food for a few days can help reduce the flare‑up, lol. Make sure you follow the doctor’s steroid eye‑drops schedule, otherwise the healing might lag. And yeah, dry eye is a big deal – using artificial tears can keep things smooth.
The inflammatory cascade post‑LASIK involves cytokine release that can impede stromal remodeling. If you’re on antihistamines, the H1 blockade may amplify vascular permeability, elevating the risk score. Moreover, isotretinoin modulates keratinocyte turnover, which could destabilize epithelial adherence. The algorithm’s weighting seems to prioritize age‑related collagen rigidity, which aligns with biomechanical studies. Ensuring a pre‑operative omega‑3 regimen could mitigate neutrophil infiltration, enhancing outcomes.
Totally agree, staying hydrated helps a lot.
Honestly, the risk calculator feels oversimplified. Reducing everything to a single score ignores patient‑specific nuances like corneal thickness. Plus, the age brackets are too broad – a 31‑year‑old isn’t the same as a 49‑year‑old. The dry‑eye binary also misses gradations that matter clinically. And the medication options leave out common NSAIDs that can affect healing. While the tool is user‑friendly, it could mislead someone into a false sense of security. I’d recommend a thorough ophthalmologist consult beyond this gimmick.
Actually, the risk score formula adds 2 points for antihistamines and omega‑3, but it should also consider dosage frequency. The script also has a typo where “age > 30 && age 50” is broken. Fixing that logic will give a more accurate output.
Post‑surgery inflammation is like a hidden storm that rages beneath the surface of our eyes after LASIK. 🌩️ When the corneal flap heals, cytokines such as IL‑1 and TNF‑α surge, orchestrating a cascade that can blur vision if not kept in check. The body’s innate immune response, while protective, can also cause excess stromal haze, which translates to visual disturbances for the patient. Age plays a pivotal role because collagen cross‑linking becomes more rigid, making the tissue less adaptable to the micro‑traumas of surgery. Dry eye, on the other hand, reduces the tear film’s lubricating capacity, allowing inflammatory mediators to linger longer on the ocular surface. Medications like isotretinoin profoundly affect keratinocyte differentiation, potentially destabilizing the epithelium after flap repositioning. Even over‑the‑counter antihistamines can dry out the ocular surface, inadvertently amplifying the inflammatory load. Omega‑3 fatty acids, however, act as natural anti‑inflammatories, shifting the balance toward resolvins and protecting the cornea. It’s fascinating how a simple dietary tweak can modulate such a complex biochemical pathway. Patients often underestimate the power of consistent post‑op eye‑drop regimens, thinking a missed dose is inconsequential. In reality, those steroid drops strategically suppress the early inflammatory wave, preventing a ripple effect that could compromise visual acuity. Moreover, compliance with follow‑up appointments allows clinicians to catch subtle signs of haze before they become permanent. The calculator’s risk stratification is a useful starting point, but it should be paired with personalized care plans. Incorporating lifestyle factors-like limiting screen time and using humidifiers-further reduces the odds of chronic inflammation. Ultimately, understanding the interplay of age, dry eye status, and medication exposure empowers patients to make informed decisions and achieve optimal LASIK outcomes. 🌟
That's a solid rundown, and I gotta say the eye‑drop schedule is non‑negotiable. If you skip a dose, the inflammation can sneak back in like a ninja. Also, keep those screens at a proper distance; blue‑light filters help. And yeah, staying on top of your meds is a game‑changer.
Good points appreciate the info
Great summary! 👍 Keep those eyes moist and follow the doctor’s orders.
The ocular immune response after LASIK is a delicate balancing act. On one side, you need enough inflammation to drive proper wound closure, but too much leads to stromal scarring. Age‑related changes in extracellular matrix composition tip this balance toward rigidity, making the cornea less forgiving. Dry eye syndrome reduces tear‑film stability, allowing inflammatory cells to accumulate. Antihistamines, while helpful for allergies, often exacerbate dryness, indirectly raising the risk. Isotretinoin’s impact on epithelial turnover is another hidden variable that patients often overlook. Omega‑3 supplements can serve as a natural anti‑inflammatory adjunct, but they’re not a cure‑all. In short, a personalized approach that weighs all these factors yields the best visual outcomes.
Look, the calculator is handy but don’t treat it as gospel. 🤨 You still need a thorough pre‑op assessment to catch hidden risks. Trust your surgeon’s expertise over a web tool.
Everyone’s experience with LASIK can vary, so it’s crucial to keep an open mind. The risk calculator gives you a baseline, but personal health history adds layers. Share your concerns with the ophthalmologist; they’ll tailor the plan. Remember, post‑op care is a partnership between you and the clinic. Stay proactive and ask questions whenever something feels off.
While the tool provides a rudimentary overview, it lacks the granularity required for a sophisticated analysis. One must consider biomechanical modeling of the corneal lamellae to truly gauge postoperative stability. Moreover, the binary classification of dry eye oversimplifies a multifactorial condition. A nuanced discussion on tear‑film osmolarity would elevate the conversation beyond superficial metrics. In essence, the calculator is a pedagogical stepping stone, not a definitive prognostic instrument.
I hear you, Kaustubh, and appreciate the deeper dive. At the same time, many patients benefit from an easy‑to‑use starting point. The calculator can spark that initial awareness, prompting them to seek detailed evaluations. It’s all about bridging the gap between lay understanding and clinical depth. Keep the dialogue inclusive, and we’ll all learn more together.
The inflammation calculator is a neat quick‑check, especially for first‑timers. It reminds you to think about meds and dry eye before diving in. Just remember it’s a snapshot, not the whole picture. Keep those follow‑up visits on schedule! 😊
Thx for the info
Alright folks, let’s get real about post‑LASIK inflammation – it’s not just a minor hiccup, it’s a full‑blown battle that can make or break your vision! You’ve got cytokines marching in, stromal cells reacting, and if you don’t keep the eye‑drops flowing, you’re basically waving a white flag. Age isn’t just a number; it’s a fortress of collagen that resists healing, so younger patients have a natural edge. Dry eye? That’s the silent saboteur, draining your tear‑film like a leaky pipe. Meds like isotretinoin are double‑edged swords – they can tone up your skin but turn your cornea into a desert. Omega‑3s are the secret weapons, rallying anti‑inflammatory troops right where you need them. The calculator gives you a risk score, but the real magic is in strict adherence to post‑op protocols. Skipping appointments? That’s a recipe for disaster. Stay hydrated, keep the screen distance, and never, ever ignore that burning sensation. Your future self will thank you for the discipline you put in today!
Honestly, this calculator is just another gimmick trying to sound scientific. It regurgitates bland stats while ignoring the messy reality of patient variability. Stop feeding us half‑baked numbers and give us real, actionable advice.