
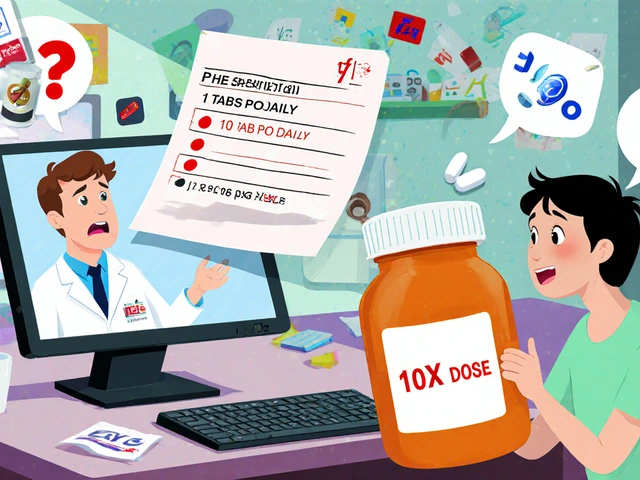
Electronic prescribing was supposed to fix the mess of handwritten scripts. No more deciphering chicken scratch. No more misreading ‘take one at bedtime’ as ‘take ten.’ But instead of disappearing, transcription errors just changed shape. Now, instead of bad handwriting, you’ve got systems talking past each other-Epic sending a script to QS/1, and the pharmacy’s software misreading ‘1 TAB PO DAILY’ as ‘10 TAB PO DAILY.’ That’s not a typo. That’s a patient risk.
Why E-Prescribing Still Causes Transcription Errors
E-prescribing cut overall prescribing errors by up to 99% in early studies. That’s huge. But here’s the catch: the errors that remain? Most of them are transcription errors. Not from doctors. Not from pharmacists. From the systems themselves.
When a doctor writes a prescription in Epic, and it gets sent to a pharmacy using a different system like Cerner or QS/1, the data doesn’t always translate. The same instruction-‘take one tablet by mouth daily’-can become ‘1 TAB PO DAILY’ in one system, and ‘1 tab po qd’ in another. Some systems interpret ‘qd’ as daily. Others? They see ‘q’ as ‘10’ and ‘d’ as ‘daily,’ and boom-you’ve got ten times the dose.
A 2023 survey from Surescripts found that 41% of pharmacists spend 15 to 30 minutes every day just fixing these mismatches. That’s not efficiency. That’s damage control.
Structured Sig Formatting Is the First Line of Defense
The most effective fix? Standardized prescription instructions-called ‘structured sigs.’ Instead of letting doctors type free text like ‘take as needed for pain,’ systems should force them to pick from a dropdown: ‘Take 1 tablet by mouth every 6 hours as needed for moderate to severe pain.’
Research from Health Affairs in 2018 showed that clinics using structured sigs reduced transcription errors by 41%. Why? Because the system knows exactly what ‘every 6 hours’ means. It doesn’t guess. It doesn’t misread abbreviations. It sends the exact instruction in a format the pharmacy system can parse.
Most ONC-certified EHRs now support this. But many providers still skip it. They’re used to typing fast. They don’t want to click through menus. Training matters. Practices that spent just 4.7 hours per provider on structured sig training saw error drops within weeks.
CancelRx: Stop the Confusion Before It Starts
One of the most common errors? A patient gets two prescriptions for the same drug. One from the ER. One from the primary care doctor. One says ‘take 5 mg daily.’ The other says ‘take 10 mg daily.’ The pharmacist sees both. Which one do they fill?
That’s where CancelRx comes in. Developed by Surescripts in 2012, CancelRx lets prescribers electronically cancel a previous prescription. No more calling the pharmacy. No more handwritten notes. No more confusion.
When a doctor changes a patient’s medication, they don’t just write a new script-they cancel the old one. The pharmacy system automatically flags the canceled script and only processes the active one. A 2021 study showed this cut discontinued medication errors by 63%.
It’s simple. But it only works if every provider uses it. And too many still don’t. They hit ‘new prescription’ and forget to cancel the old one. That’s on them. But it’s also on the system. If the EHR doesn’t make canceling easy, it won’t get done.

Single Shared Medication List: Kill the Reconciliation Errors
Patients often see multiple doctors. Each one adds a new med. None of them see what the others prescribed. So the pharmacist gets a script for a new blood pressure pill. But the patient’s current list in the pharmacy system shows three others. Which ones are still active?
A single shared medication list solves this. It’s a live, real-time list of all active prescriptions-updated across all systems. When a doctor adds a new med, it shows up everywhere. When a med is stopped, it disappears.
Practices using this feature cut reconciliation errors by 52%. One case study from MGMA showed a clinic eliminated 100% of its refill transcription errors after implementing it. That’s not luck. That’s system design.
The catch? It only works if all systems talk to each other. Epic, Cerner, QS/1, Pioneer-they all need to connect. Most don’t. That’s why standalone e-prescribing tools like DrFirst Rcopia sometimes perform better in small practices: they’re simpler, less fragmented. But integrated systems like Epic-Hyperspace cut overall prescribing errors by 84%. The trade-off? Complexity. But the payoff? Safety.
Why System Integration Beats Standalone Tools
There’s a myth that standalone e-prescribing tools are better because they’re easier to use. They’re not. They’re just less connected.
DrFirst Rcopia has 42% fewer transcription errors than EHR-integrated systems? That’s true. But only because those integrated systems are poorly configured. When Epic, Cerner, or Allscripts are properly linked to pharmacy systems using HL7 FHIR standards, transcription errors drop by 92%.
Here’s the reality: a standalone tool means the doctor writes the script, clicks send, and the pharmacy has to manually retype it. An integrated system? The script goes directly into the pharmacy’s dispensing software. No typing. No misreading. No guesswork.
That’s why fully integrated systems reduce transcription-related medication errors by 67% compared to standalone ones. The data doesn’t lie. But integration isn’t magic. It requires API compatibility, certified software, and staff training. Most small practices avoid it because they think it’s too hard. But with ONC’s 2023 Interoperability Roadmap pushing for FHIR by 2025-and $15 million in funding for small practices-it’s getting easier.

Alert Fatigue Is Making Errors Worse
Here’s something no one talks about: doctors are drowning in alerts.
‘This drug interacts with warfarin.’ ‘This dose exceeds guidelines.’ ‘Patient has renal impairment.’
They see 10, 20, 50 alerts per day. So they start clicking ‘OK’ without reading. That’s alert fatigue. And it’s causing transcription errors.
Dr. Joan Ash from Oregon Health & Science University told the FDA in 2019 that 34% of transcription errors happen because providers override warnings without checking. They’re tired. They’re rushed. They think, ‘I’ve seen this before.’ But this patient isn’t the last one.
The fix? Smarter alerts. Not more. Smarter. Only show warnings that matter. Only show them when the risk is high. And make sure the alert includes the patient’s actual lab values-not just a generic warning. A 2021 AHRQ report found that targeted alerts cut override rates by 58%.
What’s Changing in 2025?
The rules are shifting. The 21st Century Cures Act bans ‘information blocking’-meaning systems can’t block data from flowing between providers and pharmacies. Violators face fines. That’s forcing change.
And the DEA now requires all controlled substances to be e-prescribed. That alone cut transcription errors for Schedule II drugs by 57%.
But the biggest shift? FHIR. Fast Healthcare Interoperability Resources. It’s the new language all systems are supposed to speak by 2025. HL7’s Da Vinci Project showed 98% error reduction in pilot studies using FHIR for e-prescribing. That’s not a small win. That’s a revolution.
AI tools are starting to enter the picture too. Epic’s DoseMeRx, piloted in 2023, uses patient data-weight, kidney function, age-to predict safe doses. It flags mismatches before the script even leaves the doctor’s screen. Early results show a 65% drop in transcription errors from dosing mistakes.
But AI won’t fix broken systems. It’ll just make bad data look more convincing.
What You Can Do Today
You don’t need to wait for FHIR or AI to fix this. Start now.
- Use structured sigs. No free text. Pick from dropdowns. Train your team.
- Always use CancelRx. Cancel the old script before writing a new one.
- Verify the shared medication list. Before prescribing, check what’s active. Don’t assume.
- Turn off non-critical alerts. Only keep alerts that prevent serious harm.
- Ask your pharmacy: ‘Do you use FHIR?’ If they say no, push for it.
Transcription errors aren’t inevitable. They’re design flaws. And design flaws can be fixed.
It’s not about having the fanciest system. It’s about using the system right.
What are the most common transcription errors in e-prescribing?
The most common errors include misinterpreted abbreviations (like ‘qd’ read as ‘10 daily’), mismatched dosing instructions between systems, missing medication indications leading to incorrect dosing, and duplicate prescriptions that aren’t canceled. Systems that don’t use standardized sigs or shared medication lists are most prone to these errors.
Can e-prescribing systems eliminate all transcription errors?
No, not yet. While systems can reduce transcription errors by up to 92% with full interoperability and structured data, human factors like alert fatigue, poor training, and legacy system incompatibility still cause errors. The goal isn’t perfection-it’s consistent, measurable reduction through standardized workflows and system integration.
Why do some pharmacies still manually re-enter e-prescriptions?
Many pharmacies still use older systems that can’t interpret modern e-prescription formats. If the EHR and pharmacy system don’t use the same standards-like NCPDP SCRIPT 201900 or HL7 FHIR-the data arrives garbled. The pharmacy has no choice but to manually fix it. This happens in 68% of cases where systems aren’t fully integrated.
What’s the difference between standalone and integrated e-prescribing systems?
Standalone systems, like DrFirst Rcopia, let you write and send prescriptions but don’t connect to your electronic health record. That means you manually copy patient data between screens. Integrated systems, like Epic or Cerner, pull patient history, allergies, and current meds directly into the prescription screen. Integrated systems reduce transcription errors by 55% more than standalone ones when connected to pharmacy systems.
How do I know if my e-prescribing system is compliant?
Check if your system is ONC-certified for the 2015 Edition or later. It must support electronic transmission of prescriptions, include CancelRx functionality, and allow structured sig entry. Ask your vendor: ‘Do you support HL7 FHIR for pharmacy connectivity?’ If they hesitate, you’re not fully compliant-and you’re still at risk for errors.
Are there penalties for not using e-prescribing correctly?
Yes. Medicare Part D imposes financial penalties on prescribers who don’t use e-prescribing. Under the 21st Century Cures Act, systems that block data exchange can face fines up to $1 million per violation. And for controlled substances, the DEA requires electronic prescribing-paper scripts are no longer legal for Schedule II drugs.
Transcription errors aren’t going away overnight. But they’re not inevitable. Every doctor, every pharmacist, every system vendor has a role to play. Start with the basics. Use structured sigs. Cancel old scripts. Share the right data. And don’t accept a system that doesn’t talk to the next one. Patient safety isn’t a feature. It’s the only feature that matters.








Ugh, I just had a patient nearly get doubled-dosed because the system read 'qd' as '10 daily.' This isn't theoretical-it’s Tuesday morning in my clinic. 😭
Structured sigs are the quiet hero of e-prescribing. Nobody talks about them, but they’re the reason my pharmacy hasn’t called me in 8 months. Simple. Effective. Why don’t we all just use them?
Let’s be real-this whole thread is just rehashing what we’ve known since 2015. FHIR isn’t magic, it’s baseline. If your EHR can’t speak HL7 FHIR natively in 2025, you’re running a medical museum. And don’t get me started on ‘standalone’ tools-those are just glorified PDF generators with a send button. The fact that anyone still uses DrFirst Rcopia without FHIR integration is a public health liability. I’ve seen ERs where pharmacists manually transcribe scripts because the EHR vendor ‘forgot’ to enable the API. This isn’t innovation. It’s negligence dressed up as convenience.
You know, I’ve been thinking about this a lot lately-not just as a clinician, but as someone who’s watched my grandmother nearly overdose because her new cardiologist didn’t know she was already on warfarin. The systems we build aren’t just code-they’re the invisible hands holding people’s lives. And when those hands slip? It’s not a ‘mistake.’ It’s a failure of imagination. We’ve got the tech. We’ve got the data. We’ve got the standards. What we’re missing is the collective will to make it *work*-not just for efficiency, but for dignity. The fact that CancelRx exists and still goes unused? That’s not a technical problem. That’s a cultural one. We reward speed over safety. We glorify the ‘fast doc’ who clicks through alerts like a video game. But no one gets a restart button when the dose is wrong. We need to stop treating patient safety like an optional feature. It’s the foundation. Everything else is just decoration.
Use structured sigs. CancelRx. Shared med list. Done. No magic. Just discipline. If your EHR doesn’t make it easy, complain until it does. Your patient’s life isn’t a suggestion.
The interoperability gap is a structural inequity. Rural clinics with legacy systems are disproportionately burdened by transcription errors because they lack the capital to upgrade. Meanwhile, urban academic centers with FHIR-integrated Epic-Hyperspace stacks are seeing near-zero error rates. This isn’t a tech issue-it’s a policy failure. The $15M funding is a start, but it’s a Band-Aid on a hemorrhage. We need mandatory interoperability audits, not just certification checkboxes.
I love how everyone’s acting like structured sigs are some revolutionary idea. They’ve been around since 2010. The real issue? Training. And accountability. I work at a hospital where 70% of providers still type ‘take 1 tab qd’ because ‘it’s faster.’ We ran a 30-minute mandatory training last quarter. Error rates dropped 40% in two weeks. No new software. No new vendor. Just a 30-minute talk and a reminder on the login screen. Sometimes the fix isn’t tech-it’s just telling people, ‘Hey, this matters.’
As a pharmacist in Lagos, I can confirm: the issue is global. Even in low-resource settings, the same errors occur-'qd' misread, duplicate scripts, no CancelRx. The difference? We don’t have Epic or Cerner. We have paper, then a single phone call to a pharmacy that may or may not have the same drug names. Standardized sigs aren’t a luxury-they’re a lifeline. If Western systems can fix this, why aren’t we exporting the solution? Technology should serve humanity, not just hospitals with IT budgets.
Alert fatigue is real, but so is the temptation to blame the doctor. The system should adapt to the clinician, not the other way around. If a warning triggers 12 times a day for the same patient with stable creatinine, it’s not a warning-it’s noise. We need AI that learns context, not just rules. A dose warning for a 90-year-old with CKD stage 4? Fine. For a 28-year-old athlete with normal labs? Mute it. Let the system earn its beep.
It’s fascinating how we treat patient safety like a checklist item rather than a cultural imperative. We invest millions in EHRs, yet spend pennies on training. We celebrate ‘integration’ as a buzzword, but ignore the human layer-the weary resident who just worked 28 hours and clicks ‘OK’ without reading. The fix isn’t just technical. It’s ethical. We must design systems that assume human fallibility, not punish it.
AI tools like DoseMeRx? Brilliant-but only if they’re trained on diverse, real-world data. If the algorithm was trained only on data from urban academic hospitals, it’ll misjudge dosing for rural, elderly, or underweight patients. I’ve seen it happen. AI doesn’t eliminate bias-it amplifies it, if the data’s flawed. So before we cheer the ‘AI revolution,’ let’s ask: Who’s data? Whose safety? And who’s auditing the algorithm?
This is the most hopeful thing I’ve read all year. We can fix this. Not someday. Right now. Start with one thing: structured sigs. Just one. Then another. Then another. We don’t need perfection. We need progress. And progress starts with you clicking the dropdown instead of typing.
Just had a nurse say, 'I didn't know CancelRx existed.' 😅 So I showed her. 3 clicks. Done. We're gonna make a poster. 'Cancel before you create.' Simple. Love it.
One might posit that the fundamental epistemological challenge lies not in the technological architecture per se, but in the ontological dissonance between human cognitive heuristics and algorithmic determinism. The physician, operating under bounded rationality, defaults to expediency; the system, operating under syntactic precision, demands orthodoxy. The chasm between these modes is not bridged by protocol, but by cultural re-education.