
Understanding Spironolactone and Its Uses
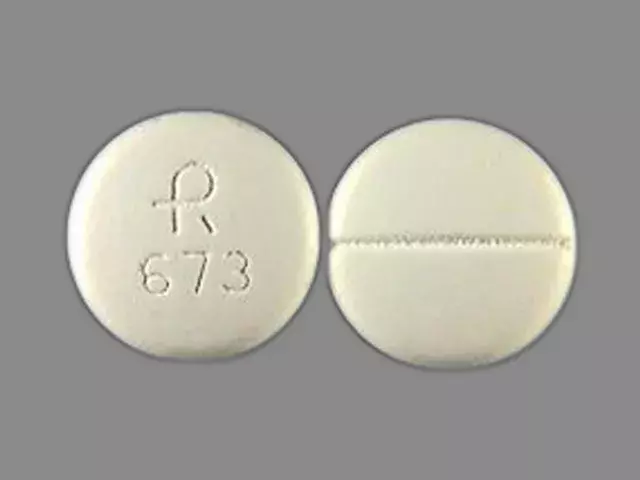
Spironolactone is a medication often prescribed to treat conditions like high blood pressure, edema, and heart failure. It is classified as a potassium-sparing diuretic and works by helping the kidneys eliminate excess water and sodium from the body. This process helps reduce the workload on the heart, ultimately lowering blood pressure and improving heart function.
Aside from its cardiovascular benefits, spironolactone is also used to treat hormonal acne and excessive hair growth in women, as it can block the effects of androgens (male hormones) in the body. As with any medication, it's essential to know how it interacts with other substances, including alcohol. In the following sections, we'll explore the potential risks and side effects of combining spironolactone and alcohol.
The Dangers of Mixing Spironolactone and Alcohol
Combining spironolactone and alcohol can lead to several adverse effects. One of the primary concerns is that both substances can cause dehydration, which can exacerbate the symptoms of low blood pressure, such as dizziness and fainting. Additionally, alcohol can interfere with the effectiveness of spironolactone, making it harder for the medication to achieve its intended purpose.
Another concern is that alcohol can increase the risk of experiencing spironolactone's side effects, such as nausea, vomiting, and diarrhea. Furthermore, alcohol consumption can also impair your judgment and ability to monitor your symptoms, which may put you at greater risk for complications.
Managing Spironolactone Side Effects
As with any medication, spironolactone may cause side effects. While some people may not experience any issues, others may encounter mild to moderate side effects that can be managed with lifestyle changes or adjustments to the medication. Some common side effects of spironolactone include dizziness, headache, stomach pain, and increased potassium levels in the blood.
To minimize these side effects, it's essential to follow your healthcare provider's instructions regarding dosage and administration. Additionally, maintaining a healthy diet, staying hydrated, and getting regular exercise can help mitigate some of the side effects associated with spironolactone. If you're concerned about the impact of alcohol on your medication, it's crucial to discuss your concerns with your healthcare provider.
Safe Alcohol Consumption While on Spironolactone
While it's generally best to avoid alcohol when taking spironolactone, it's essential to understand that everyone's tolerance and reaction to alcohol may vary. If you choose to consume alcohol while on spironolactone, it's crucial to do so in moderation and be mindful of any potential side effects or interactions. Monitoring your alcohol intake and limiting your consumption to occasional, responsible drinking can help minimize the risks associated with combining spironolactone and alcohol.
Always consult with your healthcare provider before making any changes to your alcohol consumption or medication regimen. They can provide personalized advice based on your specific circumstances and medical history.
When to Seek Medical Help
If you're experiencing severe or persistent side effects from spironolactone, it's essential to reach out to your healthcare provider for guidance. This is especially important if you suspect that alcohol may be exacerbating your symptoms or interfering with your medication. Some signs that you may need medical assistance include severe dizziness, fainting, rapid or irregular heartbeat, and signs of an allergic reaction, such as rash, difficulty breathing, or swelling of the face, lips, or tongue.
Remember, your healthcare provider is your best source of information and support when it comes to managing your health and medications. They can help determine whether spironolactone is the right choice for you and guide you in making informed decisions about your treatment plan, including how to safely navigate the relationship between spironolactone and alcohol.










People love to scare you with headlines about spironolactone and booze, but honestly the risk is overblown. The drug's diuretic effect is mild compared to alcohol's dehydrating power, and as long as you stay hydrated the combo isn’t a death sentence.
Just keep an eye on blood pressure and you’ll be fine.
That’s a good point, Timothy. 😊 I’ve read that staying well‑hydrated and monitoring how you feel after a drink are the simplest ways to avoid trouble. Also, a quick chat with your pharmacist can clear up any personal concerns.
Exactly, Kay! 🍻💊 Combining the two doesn’t have to be a disaster if you respect your body’s signals. I’ve seen patients enjoy a glass of wine occasionally without issues, as long as they don’t overdo it.
While anecdotal experiences are useful, the pharmacological basis deserves a thorough examination. First, spironolactone acts primarily on the distal convoluted tubule, reducing sodium reabsorption and conserving potassium. Alcohol, on the other hand, stimulates antidiuretic hormone release intermittently, which can paradoxically increase fluid retention in certain individuals. This interaction creates a nuanced balance: the diuretic effect of spironolactone may be blunted, leading to a modest rise in blood pressure if alcohol consumption is chronic. Moreover, both agents can precipitate orthostatic hypotension; the combined vasodilatory effect may manifest as dizziness, especially in the elderly. From a hepatic standpoint, high‑dose alcohol induces cytochrome P450 enzymes which could theoretically alter spironolactone metabolism, though clinical data remain sparse. The net result is a heightened risk of hyperkalemia, particularly in patients with compromised renal function, because alcohol can cause transient renal vasoconstriction, reducing potassium excretion. It is also worth noting that nausea and gastrointestinal upset are common side effects of spironolactone, and alcohol can exacerbate these complaints, potentially leading to poor medication adherence. In practical terms, moderation is key: limiting intake to a single standard drink per day and ensuring adequate hydration can mitigate many of these concerns. Lastly, patients should schedule regular laboratory monitoring-serum electrolytes and creatinine-when they plan to consume alcohol while on this medication. In summary, the interaction is not an absolute contraindication, but it warrants cautious, individualized management.
Great summary, Bill! I’d add that staying active and eating potassium‑rich foods like bananas can help keep levels in check. Remember, it’s all about balance.
Balance is indeed a philosophical concept applied to health. When one element overwhelms another, equilibrium is lost; thus moderation becomes the path to wellbeing.
Just don’t binge.
I totally get the concern, and the best approach is to treat this like any other medication‑food interaction: stay informed, keep a diary if needed, and talk to your doctor before making big changes.
Sounds sensible. Keep it simple.
Honestly this article feels like a rehash of basic warnings. Nothing new here.
Well, if you’re not paying attention, you might end up hurting yourself. That’s why we need to be real about these risks.
From a clinical perspective, the safest route is to schedule a brief consultation with your prescribing physician. They can assess your individual cardiovascular risk profile, review any recent electrolyte panels, and provide personalized guidance on alcohol consumption limits that align with your therapeutic objectives.
Look, nobody’s gonna police your weekend drinks, just don’t go overboard.
Mixing meds and booze can be a wild ride, but with a dash of common sense you can keep the adventure smooth.
Exactly! A little caution goes a long way, especially when you’re juggling hormones and heart health.
Yo, this is like one of those drama episodes where the hero forgets to read the fine print and ends up in a mess. Honestly, just read the label and chill, no need for a panic attack.
True that! A quick glance at the patient information leaflet can save you from a whole saga of avoidable side effects. Knowledge is power, folks.
While the layperson might dismiss a pamphlet as mere paperwork, the philosophical underpinnings of informed consent demand that we engage in a dialogue with our own bodies, interrogating each substance we introduce. The act of drinking while on spironolactone is not merely a binary choice but a spectrum of possibilities, each colored by individual metabolic pathways, genetic predispositions, and psychosocial contexts. Consequently, the decision should be framed not as a prohibition but as a mindful negotiation, where the potential for altered electrolyte balance, vasodilatory effects, and hepatic metabolism is weighed against personal lifestyle values. In doing so, we honor both the scientific rigor of pharmacology and the existential agency of the self.