
Opioid Rotation Calculator
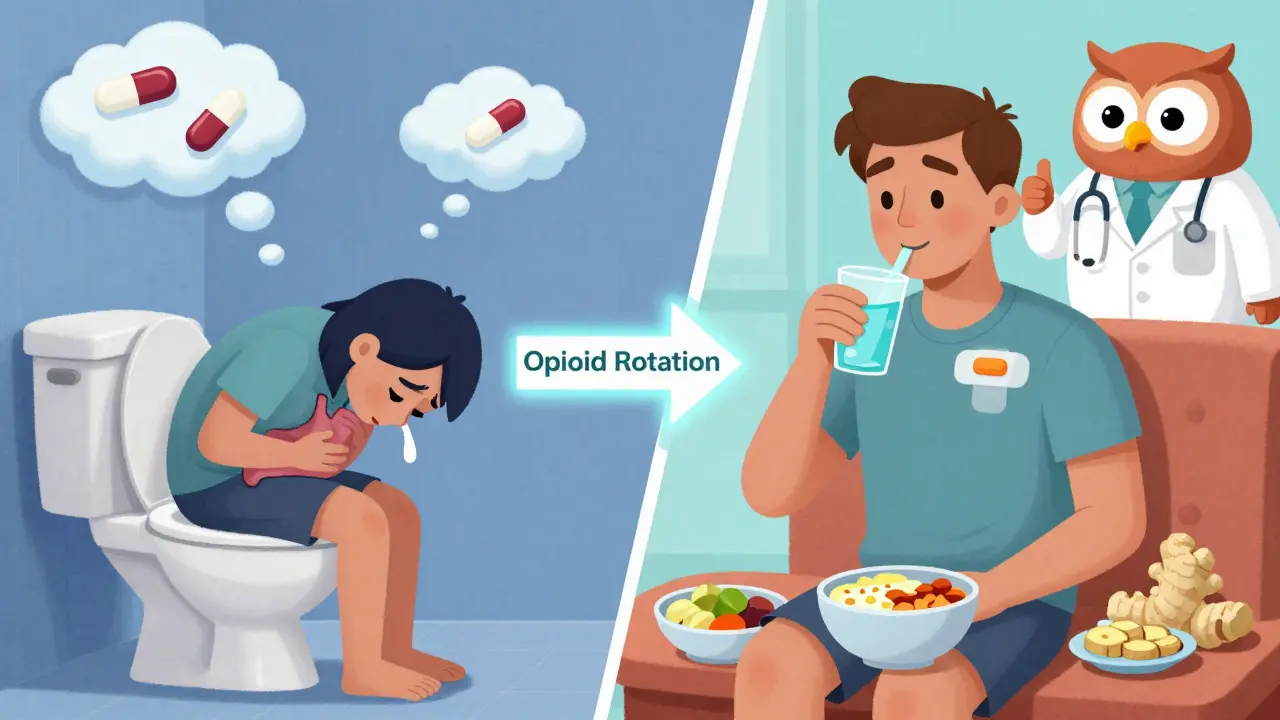
Why Rotate Opioids?
Changing opioids can reduce nausea in up to 50% of patients. This tool helps identify the best rotation options based on your current medication and nausea risk profile.
Current Opioid
Opioid Nausea Risk Profile
Oxymorphone
High nausea riskMost likely to cause nausea (up to 70% of users)
Oxycodone
Medium nausea riskModerate nausea risk
Fentanyl (patch)
Low nausea riskLeast likely to cause nausea
Morphine
High nausea riskCommonly causes nausea
Methadone
Medium nausea riskRequires careful dose adjustment
Hydrocodone
Medium nausea riskModerate nausea risk
Tramadol
High nausea riskCommonly causes nausea
Best Rotation Options
Select the opioid you're considering rotating to for nausea relief.
Fentanyl Patch
Oxycodone
Hydrocodone
Methadone
If you’re taking opioids long-term for pain and keep feeling nauseous-even after weeks or months-you’re not alone. About 1 in 3 people on chronic opioid therapy deal with persistent nausea, and for about 1 in 10, it never fully goes away. This isn’t just discomfort. It’s a barrier to pain control, sleep, eating, and daily life. The good news? There are real, evidence-backed ways to manage it-through diet, hydration, and smart medication choices. This isn’t guesswork. It’s what works based on clinical studies, patient reports, and expert protocols.
Why Opioids Make You Nauseous (And Why It Doesn’t Always Go Away)
Opioids don’t just block pain signals. They also trigger nausea through three main pathways in your body. First, they activate the chemoreceptor trigger zone in your brainstem-a spot that’s wired to vomit when it detects toxins. Second, they slow down your gut, which can cause bloating and queasiness. Third, and less known, they mess with your inner ear’s balance system. That’s why turning your head or standing up quickly can make nausea worse. This isn’t just a side effect-it’s a direct pharmacological action.
Most people develop tolerance to this nausea within 3 to 7 days. But for 15-20% of patients, it sticks around. That’s called chronic opioid-induced nausea. Why? It varies. Genetics play a role-people who are slow metabolizers of certain opioids like codeine are more likely to feel sick. The type of opioid matters too. Oxymorphone is far more likely to cause nausea than oxycodone. And fentanyl patches tend to be gentler on the stomach than oral morphine. If your nausea hasn’t improved after two weeks on a stable dose, it’s not your imagination. It’s a documented clinical issue.
Medication Options: What Works, What Doesn’t, and What to Avoid
There’s no one-size-fits-all antiemetic for opioid-induced nausea. But some options have stronger backing than others.
Metoclopramide is often the first drug doctors reach for. It speeds up stomach emptying and has about 60% effectiveness in real-world use. But it comes with a catch: long-term use can cause involuntary movements (parkinsonism or tardive dyskinesia). The FDA warns against using it beyond 12 weeks. For many, the trade-off isn’t worth it.
Prochlorperazine and promethazine (phenothiazines) are more commonly used in palliative care. Studies show they work in 65-70% of cases. They’re cheap-often under $5 a dose-and available as pills, suppositories, or injections. They can cause drowsiness, but for many, that’s better than vomiting.
Haloperidol is another option, but it’s less effective than phenothiazines-around 55% success rate-and can cause more sedation and movement issues. It’s usually reserved for when other drugs fail.
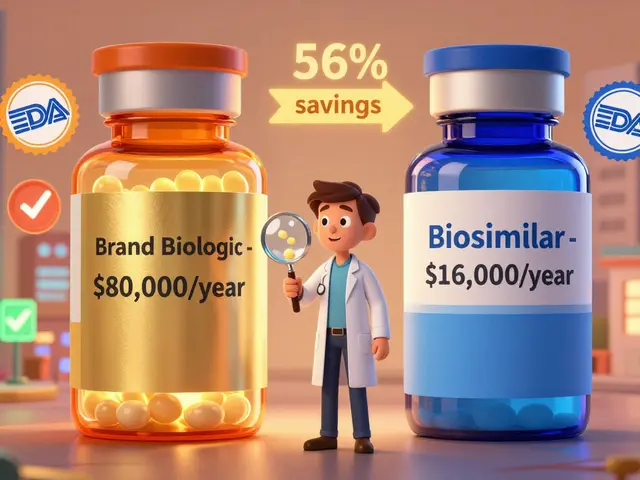
Ondansetron (Zofran) is popular because it’s well-tolerated and doesn’t cause drowsiness. But it’s expensive-up to $35 a dose-and studies show it’s no better than prochlorperazine for opioid nausea. It works better for chemotherapy-induced nausea, not opioid-related. Still, some patients swear by it for breakthrough episodes.
Dexamethasone (a steroid) helps some people, but the science is weak. It’s sometimes used in hospitals for short-term relief, but it’s not ideal for long-term use due to side effects like high blood sugar and mood changes.
There’s one emerging option: low-dose naltrexone. Early trials (like the NIH-funded study at Johns Hopkins) show that 0.5-1.0 mg daily can cut nausea severity by nearly half after 8 weeks. It’s not FDA-approved for this use yet, but some pain specialists are prescribing it off-label. It blocks the nausea-triggering effects of opioids without reducing pain relief.
Opioid Rotation: The Most Effective Strategy Many Don’t Try
If your nausea won’t quit, changing your opioid might be the single most effective step you can take. This is called opioid rotation-and it’s backed by clinical guidelines.
Switching from morphine to oxycodone can reduce nausea in up to 50% of patients. Moving from tramadol to hydrocodone or codeine helps some. Fentanyl patches are especially useful-patients in online forums report a 52% improvement in nausea after switching from oral opioids to patches. Why? Because patches deliver the drug slowly and steadily, avoiding the spikes that trigger nausea.
But you can’t just swap drugs. Methadone is different-it’s not a direct replacement. If you switch to methadone, you need to reduce your dose by 50-75% to avoid overdose. That’s because methadone builds up in your system and has a different metabolism. Always do this under medical supervision.
Studies show opioid rotation works better than adding more antiemetics. If you’ve tried three different nausea meds without success, talk to your doctor about switching opioids. It’s not giving up on pain control-it’s optimizing it.
Diet: What to Eat (And What to Avoid)
Dietary advice for opioid nausea is all over the place. Some doctors say bland foods. Some patients swear by protein. The truth? It’s personal-but patterns exist.
Forget three big meals. Instead, aim for 6-8 small meals a day, each around 150-200 calories. A 2022 survey from the University of Washington found that 55% of patients saw improvement with this approach. Why? Large meals stretch the stomach, which triggers nausea in opioid users. Small, frequent intake keeps your stomach from getting overwhelmed.
What to eat? Protein-rich snacks like hard-boiled eggs, Greek yogurt, or peanut butter on crackers came up repeatedly in patient forums. One Reddit user wrote: “I used to try crackers and toast. Felt worse. Then I started eating cheese and turkey slices. Within two days, the morning nausea faded.”
Another top recommendation: ginger. Not tea. Not supplements. Actual ginger chews. The brand Briess Ginger Chews is mentioned so often on pain forums that it’s practically a cult favorite. In one survey of 89 users, 78% reported moderate to significant relief. Ginger blocks serotonin receptors in the gut-the same ones opioids overstimulate. It’s natural, safe, and cheap.
Avoid greasy, spicy, or sugary foods. They slow digestion and worsen bloating. Cold foods often feel easier to tolerate than hot ones-steam can trigger nausea through smell. Keep snacks handy. Nausea often hits hardest in the morning or after sitting still too long.
Hydration: Sip, Don’t Gulp
Dehydration makes nausea worse. But chugging water can make it worse too.
Most clinicians say drink eight glasses a day. But patients who report success? They sip. Two to four ounces every 15-20 minutes. That’s about half a cup every 20 minutes. In a 2020 multicenter study, 47% of patients said this method reduced nausea severity. Why? Large volumes stretch the stomach and trigger the vagus nerve, which connects your gut to your brain’s vomiting center.
Electrolyte drinks like Pedialyte or low-sugar sports drinks are better than plain water for many. Opioids can cause mild dehydration through reduced fluid intake and sweating. Electrolytes help your body hold onto fluids. Avoid caffeine and alcohol-they dehydrate you and irritate the stomach.
If you can’t keep liquids down, try ice chips or popsicles. Sucking on them slowly counts as hydration. A 2021 study in the Journal of Pain and Symptom Management found that ice chips were just as effective as sipping for patients who couldn’t tolerate fluids.

The Hidden Trap: Nausea Feeds Anxiety, and Anxiety Feeds Nausea
Many patients don’t realize their fear of nausea is making it worse. This is called the nausea-anxiety cycle. You feel queasy. You worry you’ll vomit. That stress activates your nervous system, which tightens your stomach and makes nausea stronger. It becomes a loop.
Studies show that 38% of chronic opioid nausea cases are worsened by this cycle. The solution? Cognitive strategies. Try distraction-watch a show, listen to music, do a puzzle. Don’t focus on the feeling. Don’t check your stomach every five minutes. Don’t sit in the bathroom waiting for it to hit.
Also, keep your head still. Research shows that lying down with your head elevated reduces nausea by 35-40%. Closing your eyes adds almost nothing. The key is minimizing head movement. If you’re feeling sick, stay still. Don’t walk around. Don’t turn your head fast. Rest.
What’s Next? The Future of Managing Opioid Nausea
There’s real hope on the horizon. Janssen Pharmaceuticals is testing a new drug that blocks the kappa-opioid receptor-the exact pathway linked to inner ear nausea. If it works, it could prevent nausea without touching pain relief. It’s expected to hit the market around 2025.
Researchers are also looking at the gut microbiome. A 2023 study found that patients with certain gut bacteria had 32% better nausea outcomes. Future treatments might involve probiotics tailored to opioid users.
For now, though, the best tools are the ones we already have: smart opioid rotation, small meals, ginger, sipping fluids, and the right antiemetic. It’s not perfect. But it’s enough to get your life back.
What to Do If You’re Struggling
If you’ve been on opioids for more than two weeks and nausea hasn’t improved:
- Track your symptoms: When does it happen? After meals? In the morning? After moving your head?
- Try ginger chews daily-no prescription needed.
- Switch from three meals to six small ones.
- Sip fluids slowly, every 15-20 minutes.
- Ask your doctor about switching opioids-especially to a patch or oxycodone.
- If antiemetics aren’t working, ask about low-dose naltrexone (0.5-1 mg daily).
- Don’t suffer in silence. Chronic nausea is treatable. You just need the right plan.
This isn’t about quitting opioids. It’s about making them work for you-not against you.
Can opioid-induced nausea ever go away on its own?
For most people, nausea improves within 3-7 days as the body builds tolerance. But for 15-20% of long-term opioid users, it persists. This is called chronic opioid-induced nausea. It doesn’t resolve without intervention-diet changes, medication adjustments, or opioid rotation are usually needed.
Is metoclopramide safe for long-term use?
No. The FDA warns against using metoclopramide for more than 12 weeks due to the risk of tardive dyskinesia-a serious movement disorder. It’s best used short-term while your body adjusts to opioids or during a rotation. For chronic cases, phenothiazines or ginger are safer long-term options.
Why do some people get nauseated on oxycodone but not on fentanyl?
It’s about how the drug is delivered and how strongly it binds to nausea-triggering receptors. Oxycodone has a rapid peak in the bloodstream, which overstimulates the brain’s vomiting center. Fentanyl patches deliver the drug slowly and steadily, avoiding those spikes. Also, fentanyl has lower affinity for the chemoreceptor trigger zone compared to oxycodone or oxymorphone.
Can I use marijuana or CBD for opioid-induced nausea?
Some patients report relief, but there’s limited clinical data specifically for opioid-induced nausea. Cannabinoids act on different receptors than opioids, so they may help some people. However, they’re not FDA-approved for this use, and interactions with opioids aren’t fully understood. Always discuss this with your doctor before trying it.
Does drinking water help with opioid nausea?
It depends on how you drink it. Chugging large amounts can make nausea worse by stretching your stomach. Sipping small amounts-2 to 4 ounces every 15-20 minutes-helps maintain hydration without triggering the vomiting reflex. Electrolyte drinks are often better than plain water because they help your body retain fluids.
What’s the best antiemetic for opioid nausea?
For most people, prochlorperazine or promethazine work best. They’re effective in 65-70% of cases, affordable, and available in multiple forms. Ondansetron is gentler but more expensive and no more effective. Metoclopramide works but carries long-term risks. Ginger is a safe, natural option that helps many patients as a supplement or first-line choice.




I’ve been on oxycodone for 5 years and this post literally saved my life. I thought I was just weak for still being nauseous after months. Turns out, it’s not me-it’s the drug. Started sipping ginger chews and small meals every 2 hours. No more vomiting before work. Thank you for saying what doctors won’t.
Also, prochlorperazine worked better than Zofran for me. $3 vs $35? No contest.
Oh wow. So we’re now treating nausea like it’s a glitch in the Matrix? ‘Just rotate your opioid’ like it’s a firmware update? ‘Sip ginger chews’ like you’re brewing tea in a spaceship? This isn’t medicine-it’s a cult. Opioids make you sick because they’re powerful. Stop trying to hack your way out of their side effects and just accept that pain management has a cost. Maybe you don’t need opioids at all. Maybe you need to stop pretending pain is something you can out-sip with electrolytes.
Let me tell you something-nausea isn’t just a symptom, it’s a whisper from your body screaming that something’s out of alignment. Opioids? They’re like a sledgehammer to your nervous system. You think ginger chews are a band-aid? No. They’re the quiet voice that says ‘I’m still here, I still matter.’
And low-dose naltrexone? That’s not a drug-it’s a revolution. It doesn’t fight the opioid, it negotiates with it. Like a diplomat in a war zone. And the microbiome studies? We’re on the cusp of something beautiful. The gut isn’t just a pipe-it’s a second brain with its own language. And we’re finally learning to listen.
But please, stop calling it ‘chronic nausea.’ Call it ‘the body’s rebellion.’ That’s what it is. Not a side effect. A dialogue.
This is why America is falling apart. You people treat pain like a customer service issue. ‘Try this chew, sip this water, switch your drug.’ What about discipline? What about enduring? In India, we take morphine and keep working. No ginger. No sipping. Just grit. You think nausea is a problem? Try working 14 hours a day with a broken spine and no insurance. Then come back and talk about ‘optimal pain control.’
OMG YES I’VE BEEN DOING THE GINGER CHEWS AND IT’S LIKE MAGIC 🙌 I used to feel like I was gonna puke every time I sat down to eat, now I can actually enjoy my dinner without crying. Also, small meals? Game changer. I used to think I had to eat three big meals like my mom taught me-turns out my stomach is a toddler, not an adult. Also, prochlorperazine made me super sleepy but I didn’t care because I could finally sleep without feeling like I was drowning in my own guts. Thank you for writing this. I’m not alone.
ps: fentanyl patch changed my life. no more spikes. no more nausea spikes. just calm. peace.
pps: i spelled everything wrong. sorry. i’m tired.
pps: i’m crying now. not from nausea. from relief.
Metoclopramide >12 weeks = TD risk. Prochlorperazine = 65-70% efficacy. Ginger = 78% patient-reported relief. Fentanyl patch = 52% nausea reduction vs oral. Sipping = 47% improvement. Low-dose naltrexone = 50% reduction in severity. All evidence-based. No speculation. No fluff. Just data.
Stop guessing. Start optimizing.
Wait so… you’re telling me I don’t have to just suffer through this? Like… I could actually feel better? I thought this was just part of the ‘you’re on opioids now, enjoy your nausea’ package. I’ve been taking morphine for 3 years and thought I was broken. Turns out I just needed to sip water like a civilized person and eat cheese. I feel like I’ve been living in a horror movie and someone just turned on the lights.
Also, ginger chews? I bought a bag. I’m eating them like candy now. No regrets.
I want to thank the person who wrote this. Not just for the facts, but for the tone. You didn’t shame people for still being sick after weeks. You didn’t say ‘just tough it out.’ You didn’t pretend this was simple. You showed up with science and kindness. That’s rare.
To anyone reading this and feeling like a burden: you’re not. Your body isn’t failing you. The system is failing you. And you deserve better than silence.
Start with ginger. Start small. You’ve already survived 100% of your worst days. Keep going.
I used to think I was weak because I couldn’t handle the nausea. I’d force myself to eat, I’d push through, I’d cry in the bathroom while my kids played outside. Then I tried ginger chews. Didn’t work at first. Then I started sipping. Then I switched to oxycodone. Then I started eating protein snacks. And one day-I didn’t feel sick. Not even a little.
This isn’t about being ‘strong.’ It’s about being smart. And I’m so mad I didn’t know this sooner. But now I do. And I’m telling everyone. You’re not broken. You’re just waiting for the right info. And now you have it.
Don’t give up. I didn’t. And I’m still here.
Typical American medical nonsense. You’re telling people to sip water and eat cheese instead of prescribing real drugs? This is why we have a crisis. People need strong antiemetics, not snack schedules. If you can’t handle opioids, don’t take them. End of story.
ginger chewz r so goood. i tried them after reading this. no more puking in morning. thank u. also sipping water like 1 sip every 15 min. its weird but works. i dont know why doctors dont tell us this.
Let’s think beyond the pharmacology. Opioid-induced nausea isn’t just a physiological event-it’s a metaphysical rupture. The body, once a vessel of resilience, now becomes a battleground between the will to endure and the instinct to reject. We are not merely patients-we are witnesses to the paradox of modern pain management: the very substance that silences suffering becomes the architect of new torment. The ginger chew? It is not a cure. It is a ritual. A quiet act of rebellion against the tyranny of chemical inevitability. And the sipping? It is mindfulness in liquid form. Each drop, a prayer. Each swallow, a reclamation. We are not treating nausea. We are relearning how to inhabit our bodies after they’ve been colonized by synthetic grace.
Ken, you’re right that some people need stronger meds. But dismissing dietary and behavioral strategies as ‘cheese and sipping’ ignores the lived reality of millions. I’ve seen patients on high-dose fentanyl who still feel nauseous-and they’re terrified. They’re not lazy. They’re not weak. They’re just stuck in a system that doesn’t listen. This post gave them tools. Tools that cost nothing. Tools that don’t add side effects. That’s not nonsense. That’s justice.