
Decongestant Safety Checker
Check if Decongestants Are Safe For You
Answer a few questions about your heart health to see if decongestants are safe for you.
If you have heart disease or high blood pressure, taking a common cold medicine could be riskier than you think. Decongestants like pseudoephedrine and phenylephrine are in nearly every over-the-counter cold and flu remedy. They work fast-your nose clears up in minutes. But that relief comes with a hidden cost for your heart. These drugs don’t just shrink swollen nasal passages. They tighten blood vessels all over your body. And for someone with heart disease, that can mean trouble.
How Decongestants Affect Your Heart
Decongestants are alpha-adrenergic agonists. That’s a fancy way of saying they mimic adrenaline. When you take them, your body reacts like it’s under stress. Your blood vessels constrict. Your heart beats faster. Your blood pressure rises. For a healthy person, this might be barely noticeable. For someone with heart disease, it’s like pouring gasoline on a fire. Pseudoephedrine, the active ingredient in Sudafed, has been studied extensively. A 2005 meta-analysis found that even standard doses caused a small but measurable spike in systolic blood pressure-about 1 to 3 mm Hg on average. Sounds minor, right? But in someone with uncontrolled hypertension, that little jump can push blood pressure into dangerous territory. One case documented a 5-year-old girl developing high blood pressure after just four days of prescribed phenylephrine. Her pressure returned to normal only after stopping the drug. Topical nasal sprays like oxymetazoline (Afrin) and naphazoline are often seen as safer because they’re applied locally. But they’re not risk-free. A study of 100 patients showed their heart rates climbed significantly after a week of use. And there’s a documented case of a 40-year-old man who went into heart failure after overusing naphazoline nasal spray. He didn’t have a history of heart problems. He just used more than recommended. The result? Life-threatening complications.Who’s at the Highest Risk?
Not everyone with heart disease needs to avoid decongestants completely. But some groups are in serious danger:- Uncontrolled high blood pressure - Even a small rise can trigger a stroke or heart attack.
- Heart failure - Decongestants make the heart work harder when it’s already struggling.
- History of heart attack or stroke - Your arteries are already damaged. Constriction increases the chance of another event.
- Arrhythmias - Decongestants can trigger dangerous irregular heartbeats, including ventricular tachycardia.
- Prinzmetal angina - This rare condition causes coronary artery spasms. Decongestants can make those spasms worse.
Why Over-the-Counter Doesn’t Mean Safe
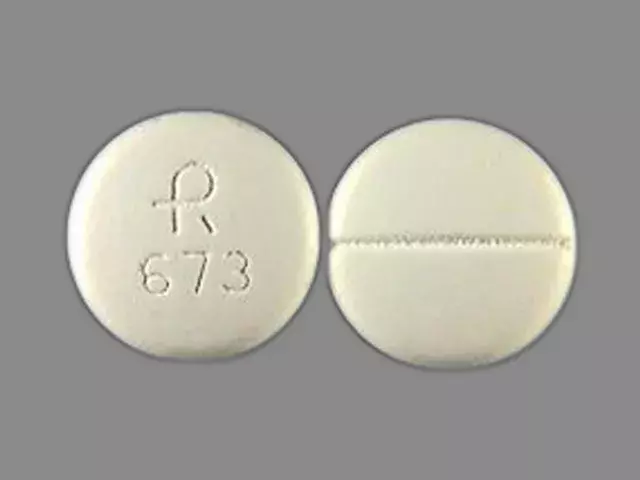
Many assume that because decongestants are sold without a prescription, they’re harmless. That’s a dangerous myth. Pseudoephedrine is kept behind the pharmacy counter in the U.S. and Australia for a reason. Pharmacists are trained to ask questions: Do you have high blood pressure? Are you on heart medication? Have you had a heart attack? These screenings exist because the risks are real. Even products labeled "heart-safe" or "for high blood pressure" often contain phenylephrine instead of pseudoephedrine. But studies show phenylephrine still raises blood pressure-just less predictably. And topical sprays? They come with the same warnings on the label. Most people never read them. The European Journal of General Medicine puts it bluntly: decongestants offer only temporary relief. They don’t cure the cold or allergy. And for people with heart disease, the downsides far outweigh the benefits.
What to Use Instead
You don’t need decongestants to feel better. Here are safer, proven alternatives:- Saline nasal spray - Flushes out mucus without affecting blood pressure. Can be used multiple times a day.
- Humidifiers - Moist air reduces nasal swelling naturally. Especially helpful at night.
- Guaifenesin (Mucinex) - Thins mucus so you can clear it easier. No effect on blood pressure or heart rate.
- Steam inhalation - A bowl of hot water with a towel over your head can open nasal passages safely.
- Rest and hydration - Your body heals faster when it’s not stressed. Drink water. Sleep. Avoid caffeine and alcohol.
The Bigger Picture: Illness Itself Strains Your Heart
It’s not just the decongestant. Having a cold or flu puts extra stress on your cardiovascular system. Your heart rate goes up. Inflammation spreads. Your body is fighting an infection while trying to keep your blood pumping. That’s hard on a weak heart. A 2017 study of nearly 10,000 heart attack patients found they were more than three times as likely to have another heart attack within a week if they took NSAIDs like ibuprofen while sick. Decongestants aren’t NSAIDs, but they add to the same kind of strain. So even if you skip the decongestant, you still need to be careful with other meds and rest properly.
What to Do If You Already Took a Decongestant
If you have heart disease and accidentally took a decongestant, don’t panic. But pay attention:- Check your blood pressure if you have a home monitor.
- Watch for chest pain, dizziness, rapid heartbeat, or shortness of breath.
- Stop taking it immediately.
- Contact your doctor or pharmacist if symptoms develop.
Final Takeaway: Your Heart Comes First
Decongestants aren’t evil. They work. But they’re not for everyone. If you have heart disease or high blood pressure, the safest choice is often no decongestant at all. The relief is temporary. The risk isn’t. Read every label. Ask your pharmacist. Choose alternatives that don’t tighten your blood vessels. Your heart will thank you.Can I take pseudoephedrine if my blood pressure is controlled?
Even if your blood pressure is controlled, pseudoephedrine can still cause a rise in pressure and increase heart rate. Most doctors recommend avoiding it entirely if you have heart disease. Safer alternatives like saline spray or guaifenesin are preferred. If you must use it, talk to your doctor first and monitor your blood pressure closely.
Are nasal sprays safer than pills for people with heart disease?
Topical nasal sprays like oxymetazoline are often thought to be safer because they act locally. But they still enter the bloodstream, especially with overuse. Studies show they can raise heart rate and, in rare cases, trigger severe high blood pressure or heart failure. They’re not risk-free. Limit use to 3 days max and avoid if you have uncontrolled hypertension or heart failure.
What cold medicines are safe with heart disease?
Safe options include saline nasal sprays, humidifiers, guaifenesin (for mucus), and acetaminophen (for fever or pain). Avoid multi-symptom products that combine decongestants with antihistamines or pain relievers. Always check the active ingredients. If it says "decongestant," "pseudoephedrine," or "phenylephrine," skip it.
Why is phenylephrine still sold if it raises blood pressure?
Phenylephrine replaced pseudoephedrine in many products after pseudoephedrine was restricted due to methamphetamine production. But research shows phenylephrine is less effective as a decongestant and still raises blood pressure in some people. It’s still available because it’s not banned-just less effective. For people with heart disease, neither is recommended.
Can decongestants cause a heart attack?
Yes, in rare cases. Decongestants can trigger heart attacks in people with coronary artery disease by constricting blood vessels that supply the heart. There are documented cases of heart attacks following use of nasal sprays and oral decongestants, especially when taken in high doses or by people with existing heart conditions. The risk is low for healthy people but significant for those with heart disease.






Seriously? I just took Sudafed yesterday and I'm fine. 🤷♀️ Why do we turn every little thing into a medical emergency? My grandma took this stuff for 40 years and lived to 92. 🍎
The assertion that decongestants pose a clinically significant risk to individuals with controlled hypertension is not supported by the most recent meta-analyses. The American Heart Association's advisory, while well-intentioned, lacks granularity regarding dosage thresholds, pharmacokinetic variability, and comorbid pharmacotherapy interactions. One must exercise rigorous scientific skepticism before endorsing blanket contraindications.
i read this and was like wait so phenylephrine is bad too?? i thought it was the safe one?? lol i always pick the 'heart safe' ones cause i have high bp but now im scared 😬
There’s a quiet tragedy in how we treat illness like a battlefield to be won with chemicals. We reach for the quick fix-decongestants, NSAIDs, stimulants-because we’re too tired to sit with discomfort. But the body doesn’t need more force. It needs space. Humidity. Rest. Water. The cold doesn’t need to be conquered; it needs to be witnessed. And sometimes, the bravest thing you can do is nothing at all.
This article is just fearmongering. Pharma companies don't want you using cheap OTC meds. They want you paying for expensive alternatives. Also, why is this even a thing? People have been taking Sudafed since the 1950s. If it was that dangerous, we'd have millions dead by now.
I got a cold last winter and skipped the decongestants. Just drank tea, slept a ton, and used a humidifier. Felt better after 4 days. No panic, no BP spikes. Honestly? The body knows what to do if you just let it.
yo i been usin Afrin for like 3 weeks straight cause my nose is always clogged. i thought it was fine since it's just a spray. now i'm like... wait did i just give myself a heart attack? 😳
I used to think 'natural' meant 'weak.' Then I got sick after my bypass and tried the saline spray. I cried. Not from the sniffles. From the relief-real, quiet, no-jitter, no-panic relief. My heart didn't have to fight the medicine. It just had to rest. That's the difference between healing and hacking.
This is the kind of info that saves lives. Seriously. I'm a nurse and I've seen three patients in the ER over the past year because they thought 'it's just a cold medicine.' Don't be that person. Ask your pharmacist. Bring your meds. Your heart isn't just a pump-it's your life.
They banned pseudoephedrine because of meth. Now they're lying about phenylephrine being safe. Big Pharma doesn't care if your heart fails. They just want you buying their new 'heart-safe' bottle with a bigger price tag. Wake up.
I read this and immediately checked my medicine cabinet. Found three bottles with 'decongestant' in the ingredients. One was labeled 'for high blood pressure.' I threw them all out. No regrets.
The most important takeaway isn't which drug to avoid-it's that you should always consult a pharmacist before taking any OTC medication if you have cardiovascular disease. Pharmacists are trained to spot interactions, and they're often more accessible than your primary care provider.