
Imagine you’ve just polished off your favorite spicy meal. That familiar, fiery feeling creeps up your throat, and within minutes, you’re deep in the kitchen cabinet, searching for relief. For millions, recurrent acid reflux and heartburn isn’t just an inconvenience—it’s a daily reality. And for many, the real game-changers aren’t antacids, but something way more advanced: proton pump inhibitors (PPIs). These drugs have swept through clinics over the past 30 years, offering long-lasting relief for stubborn stomach acid problems. But how do they actually work? And with all the choices out there—omeprazole, pantoprazole, esomeprazole, and more—how do you know which one is right for your body and your situation? There are subtle but significant differences. So let’s break them down and make sense of the science, without the mind-numbing jargon.
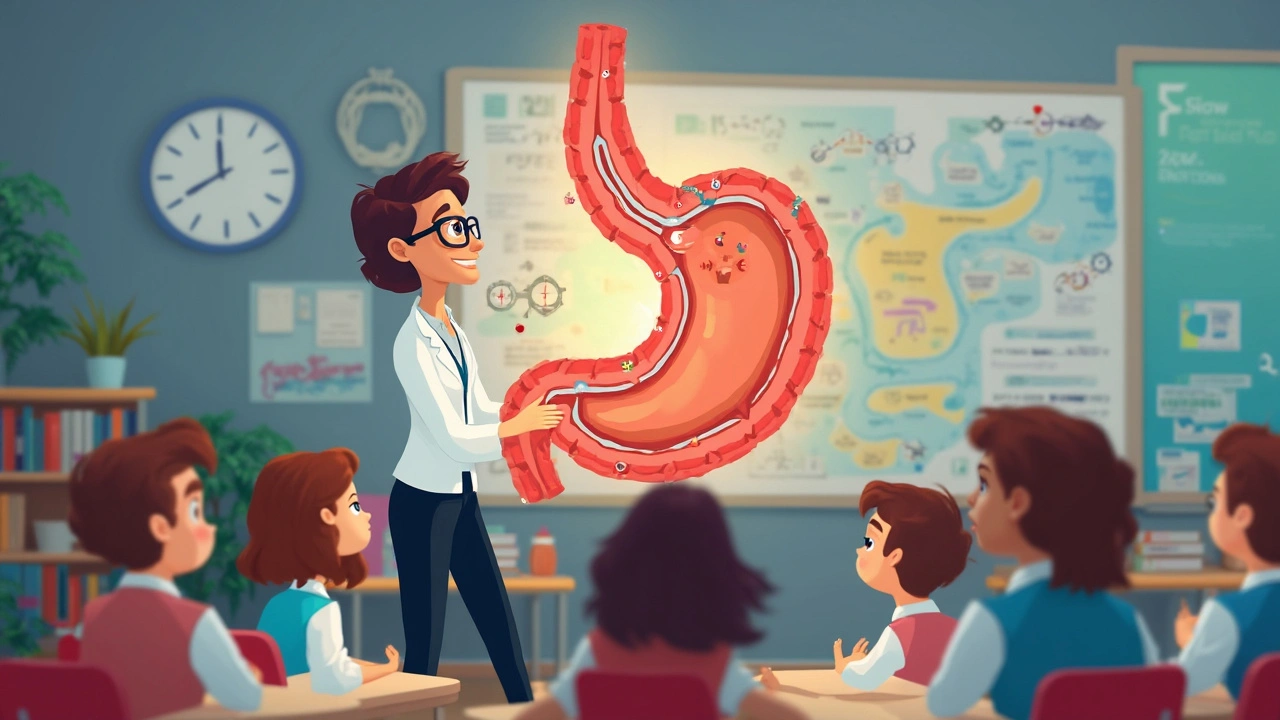
How Proton Pump Inhibitors Work: The Pharmacology Behind PPI Magic
If you zoomed in on the lining of your stomach, you’d find tiny, specialized cells called parietal cells. They’re like the factory workers in charge of making stomach acid. Inside these cells are molecular machines called proton pumps. Think of them as little acid cannons, firing hydrogen ions (protons) into your stomach to keep things running acidic and efficient, especially after a big meal.
Proton pump inhibitors zero in on these acid cannons directly. Instead of blocking acid after it’s already made, PPIs go straight to the source. They bind irreversibly to a specific enzyme—H+/K+ ATPase—embedded in the membrane of those parietal cells. Once attached, the pump is out of commission until your body makes new ones, which takes 24-48 hours. So with a single daily pill, you dramatically lower acid production for up to 24 hours. That’s why PPIs last so much longer than regular antacids or H2 blockers.
This brings serious benefits for people struggling with chronic acid reflux, peptic ulcer disease, Zollinger-Ellison syndrome, and even some cases of persistent heartburn. Without all that extra acid splashing around, the esophagus can finally start healing, and those fiery symptoms settle down. Studies show that PPIs can heal erosive esophagitis in up to 80% of cases within 8 weeks—a huge leap compared to earlier treatments. This isn’t just symptom control—it’s repairing real damage.
There’s also an interesting scientific tidbit: PPIs are actually prodrugs. This means the pill you swallow is inactive. It gets absorbed into your bloodstream and is only activated by the acidic environment right by the parietal cell pumps. That’s why you’re always told to take PPIs 30-60 minutes before eating—the food triggers more pump activity, drawing the drug right to the spots where it’s needed most. Skipping this timing step can seriously lower how well PPIs work, so don’t brush it off. Always plan that dose before breakfast; your stomach will thank you.
When and Why to Use PPIs: Indications That Go Beyond Heartburn
PPIs are best known for tackling acid reflux and heartburn, but their uses are way broader. If you scan through medical guidelines, you’ll see them recommended for:
- Gastroesophageal reflux disease (GERD): The go-to choice for moderate to severe cases, especially when symptoms stick around despite lifestyle changes or antacids.
- Erosive esophagitis: When reflux isn’t just annoying, but damaging tissue. PPIs are considered frontline for healing these erosions quickly and keeping them from coming back.
- Peptic ulcer disease: Including ulcers linked to Helicobacter pylori infection or NSAID use. PPIs help ulcers heal and, when combined with antibiotics, can even help kill off H. pylori for good.
- Zollinger-Ellison syndrome: A rare condition where tumors force the stomach to churn out excessive acid. Here, high-dose PPIs are a lifeline.
- Prevention of NSAID-induced ulcers: People on chronic NSAIDs (think long-term pain management) need stomach protection, and this is where PPIs shine.
- Laryngopharyngeal reflux and Barrett’s esophagus: Emerging research supports PPIs in these tougher cases—where acid sneaks up even into the throat or changes the lining of the esophagus at a cellular level.
Doctors don’t just throw PPIs at every bit of heartburn. They weigh a bunch of factors: symptom duration, presence of alarm signs (bleeding or trouble swallowing), and whether over-the-counter remedies do the trick. Some guidelines suggest limiting use to 8 weeks unless there’s a clear reason to keep going. Long-term users should check in with a doctor regularly, as being on these meds for years can sometimes kick up side effects like lower magnesium, vitamin B12 deficiency, or more rarely, a risk of fractures. It’s not doom and gloom—just a reminder that, like all strong tools, PPIs are best used thoughtfully.
One other thing a lot of folks don’t realize: PPIs don’t work instantly. Unlike antacids, which can take the edge off burning in minutes, PPIs can take 1-4 days to hit their full stride. So hang tight, stick to the plan, and don’t be tempted to double up in frustration. Consistency wins this race.
Comparing PPIs: Omeprazole, Pantoprazole, Esomeprazole, and More
The pharmacy shelf seems crowded with choices: omeprazole, esomeprazole, pantoprazole, lansoprazole, rabeprazole, and dexlansoprazole. On the surface, they all look about the same—they’re all proton pump inhibitors, after all. But if you talk to a gastroenterologist, you’ll hear about subtle but meaningful differences.
Here’s a quick snapshot of what each brings to the table:
| PPI Name | Brand Examples | Usual Dosing | Food Interactions | Notable Facts |
|---|---|---|---|---|
| Omeprazole | Prilosec | 20-40 mg daily | Take before meals | First widely used PPI; can interact with some blood thinners |
| Pantoprazole | Protonix | 40 mg daily | Less affected by food | Less likely to cause drug interactions |
| Esomeprazole | Nexium | 20-40 mg daily | Take before meals | "S-enantiomer" of omeprazole; slightly higher blood levels |
| Lansoprazole | Prevacid | 15-30 mg daily | Take before meals | Dissolvable forms available |
| Rabeprazole | AcipHex | 20 mg daily | Take before meals | Often used for quick symptom control |
| Dexlansoprazole | Dexilant | 30-60 mg daily | No timing issues with meals | Dual-release design, helpful for nighttime symptoms |
So, how do you choose? For most people, it comes down to personal factors: insurance coverage, how you respond, and, rarely, sensitivity to drug interactions. Omeprazole is often first-line because it’s cheap and familiar, but, being an older drug, it’s more likely to interact with meds like clopidogrel (an antiplatelet). Pantoprazole is a frequent substitute for patients on blood thinners or with concerns about interactions. Esomeprazole and dexlansoprazole can offer a little edge in symptom control or convenience, but generally, you won’t see wild differences in long-term results from one to the next.
Here’s the twist: not everyone reacts identically. Genetics can affect how you metabolize these drugs (thanks to some quirks in liver enzyme CYP2C19), which means two people, on the same dose, can get different results. So if you’re not getting relief from one PPI after a few weeks, it’s totally legit to try another—it’s not about brand loyalty, it’s about what works for your digestive system.
If you’re weighing pantoprazole vs omeprazole, check out that side-by-side comparison for more nitty-gritty details. Some patients swear one is gentler or works faster than the other, and there are real data points behind those anecdotes—like how pantoprazole’s lower risk of drug interactions makes it a winner for folks on multiple medications.
Another handy tip: If you suffer with nighttime reflux, PPIs like dexlansoprazole, thanks to their dual-release formula, can tackle symptoms that pop up after dinner or before bed. That’s not marketing fluff; those extended-release designs genuinely smooth out acid suppression over a full 24-hour cycle.
Maximizing Benefits and Avoiding Pitfalls: Smart PPI Use in Real Life
High hopes and high stakes. That’s what comes with using the most potent acid blockers science has ever cooked up. But like any powerful fix, smart use means knowing where the potholes are and how to steer clear.
Let’s hit the need-to-knows:
- Time it right. Always take your PPI about 30-60 minutes before breakfast—your stomach’s most active time for acid production. If you miss the window, wait until the next day. Doubling up won’t speed results.
- Taper when possible. Heavy, long-term use can cause rebound acid hypersecretion if stopped suddenly. Always talk to your doctor about tapering, especially if you’ve been on a PPI daily for more than a few months.
- Watch for subtle side effects. Low magnesium, low B12, increased risk of C. diff infections—most people will never notice, but if you’re using PPIs for months or years, it’s smart to get annual labs and bring up any strange symptoms (muscle cramps, tingling, or recurring diarrhea).
- PPIs vs antacids/H2 blockers. PPIs give full-strength, long-term acid control. For quick symptom relief or for mild cases, antacids (like Tums) or H2 blockers (like famotidine) might be enough, or even great to use as needed alongside your PPI, especially when weaning down.
- Don’t ignore the basics. Even with a strong PPI, simple changes—like raising the head of your bed, cutting late-night snacks, or ditching trigger foods—can make a huge difference. Drugs and lifestyle aren’t either/or; together they’re unstoppable.
- Flag any serious symptoms. Bloody stool, trouble swallowing, vomiting blood—these are red flags that always need a doctor’s attention, PPI or not.
And just a reminder: Kids and pregnant women have special considerations. Always get medical advice for these groups. Not all PPIs are approved in younger children, and only certain ones are considered safe in pregnancy.
As for buying PPIs, price varies wildly—some are dirt cheap over-the-counter, others (like esomeprazole or dexlansoprazole) can cost more. Generics work just as well as brand-name for most folks. The real power is in consistency and getting the timing right.
For those nerding out on data, here’s a quick comparison of onset, duration, and metabolism of the main PPIs:
| PPI | Onset of action | Peak effect | Metabolism pathway | Renal dose adjustment? |
|---|---|---|---|---|
| Omeprazole | 1 hour | 2-3 hours | CYP2C19, CYP3A4 | No |
| Pantoprazole | 2.5 hours | 2-3 hours | CYP2C19, CYP3A4, sulfation | No |
| Esomeprazole | 1-2 hours | 1.5-2 hours | CYP2C19, CYP3A4 | No |
| Lansoprazole | 1.7 hours | 1-3 hours | CYP2C19, CYP3A4 | No |
Proton pump inhibitors have revolutionized acid suppression therapy, but that doesn’t mean bigger doses or lifelong prescriptions are the answer for everyone. Talk with your healthcare provider about your unique history, and if your plan includes a PPI, get curious—ask questions, notice how your body responds, and keep the lines open.
The best part? Understanding these meds puts you in control. No more guessing, no more one-size-fits-all solutions. You get to team up with your doctor, dial in the best plan, and—maybe, just maybe—enjoy that next fiery dinner with a little less worry and a lot more flavor.






Taking a PPI the right way can feel like a small ritual, but it really does make a big difference. The 30‑60 minute window before breakfast lets the drug hit the active pumps when they’re most engaged. Consistency also helps prevent the rebound acid surge you sometimes see after stopping abruptly. If you ever miss a dose, just skip it and resume the next day rather than doubling up. Keep an eye on any new symptoms like muscle cramps or tingling, and bring them up at your next check‑up.
Wow, this whole PPI deep‑dive is like a blockbuster movie for my gut! 🎬 The way you explained the pro‑drug activation had me picturing tiny secret agents sneaking into the stomach. And the table of drug differences? Pure gold. I’m definitely switching to the dual‑release dexlansoprazole for those midnight fire‑breathers. 🔥💊
Honestly, most of this article reads like a cheerleading script for pharma. The “magic” language masks the fact that long‑term PPI use can deplete magnesium and B12, yet you barely mention the risk. And the claim that PPIs heal 80 % of erosive esophagitis in eight weeks is cherry‑picked data; many trials show a far lower real‑world success rate. Readers deserve a harsher reality check.
🚨 drama alert 🚨 swooping in to remind everyone that “magic” has a price tag – the cost, the side effects, the rebound. 🎭 you’ve got the hype but forget the nuance. 🤷♂️
The variability in CYP2C19 activity means two patients on the same omeprazole dose can see completely different acid suppression. Poor metabolizers often achieve higher plasma levels, which can improve symptom control but also raise the risk of drug interactions. Conversely, rapid metabolizers may need a higher dose or a switch to pantoprazole, which relies less on that pathway.
In the contemporary therapeutic landscape, proton pump inhibitors occupy a position of unparalleled prominence, having supplanted older H2 antagonists in the management of acid‑related disorders. Their mechanism of action, predicated upon irreversible inhibition of the gastric H⁺/K⁺‑ATPase, confers a duration of effect that extends well beyond the pharmacokinetic half‑life of the parent compound. Consequently, a single daily dose may sustain acid suppression for up to twenty‑four hours, a fact which behooves clinicians to schedule administration in the pre‑prandial window. It is noteworthy that the pro‑drug nature of these agents necessitates activation within the acidic milieu of the secretory canaliculi, thereby rendering timing critical for optimal efficacy. Moreover, inter‑individual variability, largely attributable to polymorphisms in the CYP2C19 enzyme, engenders a spectrum of metabolic capacities ranging from ultra‑rapid to poor metabolizers. This genetic heterogeneity not only influences plasma concentrations but also modulates the probability of adverse effects such as hypomagnesemia or vitamin B12 deficiency. While the literature extols the success of PPIs in promoting mucosal healing, it concurrently documents an increased incidence of Clostridioides difficile infection among long‑term users, a phenomenon which warrants vigilant surveillance. In addition, epidemiologic investigations have raised concerns regarding a modest elevation in fracture risk, particularly in the elderly population, ostensibly linked to impaired calcium absorption. The clinical decision‑making process, therefore, must balance the undeniable therapeutic benefits against these potential iatrogenic complications. It is incumbent upon the prescribing practitioner to reassess the necessity of continued therapy at regular intervals, typically after an eight‑week trial period, unless compelling indications dictate prolonged use. Furthermore, tapering strategies should be employed to mitigate rebound hypersecretion upon cessation, a protocol that often involves gradual dose reduction or transition to an H2 blocker. The emergence of dual‑release formulations, such as dexlansoprazole, offers a pharmacologic innovation aimed at addressing nocturnal acid breakthrough, yet their cost‑effectiveness remains a point of contention. When considering drug‑drug interactions, omeprazole’s propensity to inhibit CYP2C19 must be weighed against concomitant agents like clopidogrel, where reduced activation may attenuate antiplatelet efficacy. On the contrary, pantoprazole exhibits a more favorable interaction profile, rendering it a suitable alternative in polypharmacy contexts. Ultimately, the selection of a specific PPI should be individualized, taking into account genetic factors, comorbid conditions, insurance formularies, and patient preference. By integrating these considerations, clinicians can optimize therapeutic outcomes while minimizing inadvertent harm.
What a spectacular showcase of science!!! 🎉 The way you broke down each PPI feels like a culinary tasting menu for the stomach!!! 🍽️ From omeprazole’s classic charm to dexlansoprazole’s dual‑release fireworks, every option is highlighted with such sparkle!!! ✨ Keep the tables coming, they are the real MVPs!!! 🙌
Reading this made me feel less alone in my reflux journey 😊 Knowing there are clear guidelines and options gives a boost of confidence. Remember to pair the medication with simple lifestyle tweaks – like elevating your head while sleeping and avoiding late‑night meals.
Take care of yourself, and don’t hesitate to reach out to a gastroenterologist if you notice any warning signs. 🌟
Short‑term PPI use is generally safe if you follow the doctor’s instructions.
Just to clarify, the article mistakenly says PPIs “heal 80 % of erosive esophagitis in eight weeks,” but the cited studies actually report a range of 60‑70 % depending on the cohort. Precision matters when we discuss clinical outcomes.
It’s great to see so many perspectives shared here – from the science nerds to the daily sufferers. Remember, whatever PPI you end up on, you deserve support and respect from both your health‑care team and your community. Let’s keep the conversation open and welcoming for anyone seeking advice.
yeah but you cant just rely on meds they want to know real life hacks dont they
Look lads, if the pharma giants push these drugs worldwide, you better trust local doctors who know the real impact on our Irish health system. No need for foreign hype.
For anyone considering switching PPIs, a practical tip is to keep a simple diary of your symptoms, timing of doses, and any side effects. After a week, compare the scores – lower numbers mean better control. This approach can help you and your doctor decide whether a dose adjustment or a different agent is warranted. Also, remember that generic omeprazole and its brand counterpart are therapeutically equivalent, so cost‑saving is possible without sacrificing efficacy.
Team, let’s harness the pharmacodynamics of H⁺/K⁺‑ATPase inhibition and implement a titration protocol that syncs with your circadian acid peaks. By aligning the PPI dosing schedule with the hormonally driven gastric phase, you’ll maximize the area under the curve and minimize rebound acidity. Stay proactive, track your biomarkers, and you’ll dominate reflux like a pro!