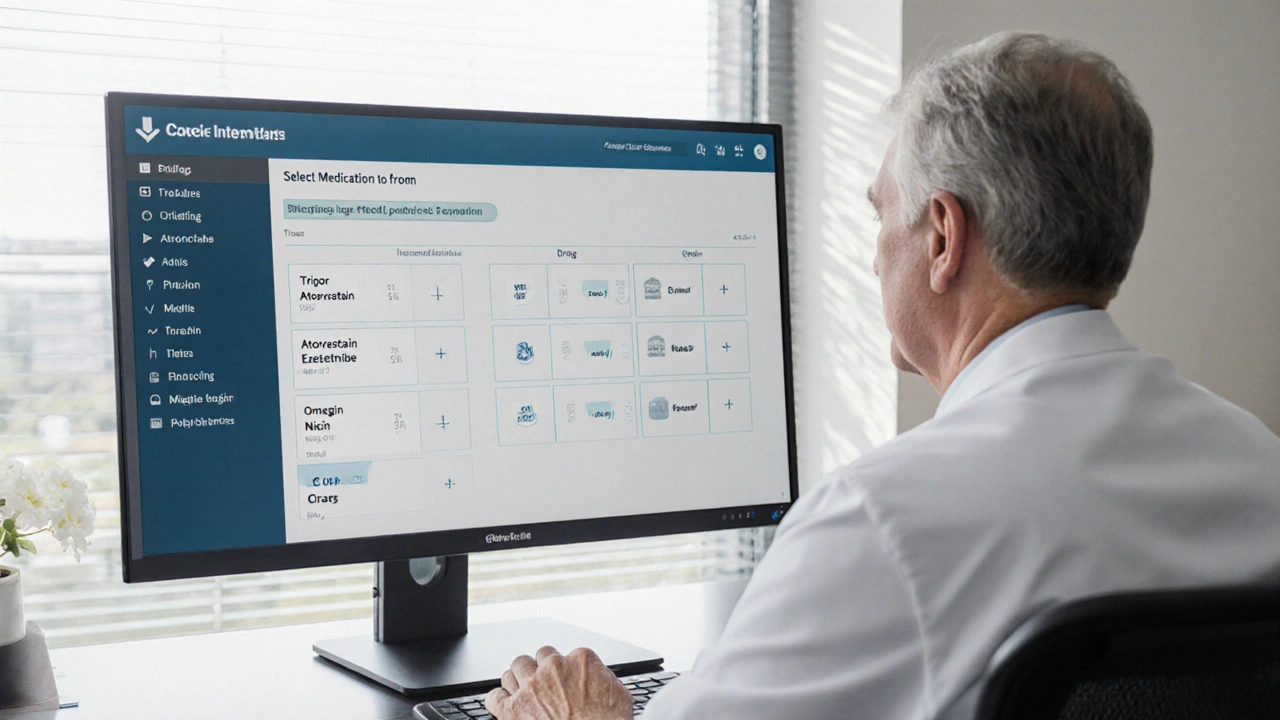
Tricor vs. Other Lipid-Lowering Medications Comparison Tool
Tricor (Fenofibrate)
Primary Target: Triglycerides ↓, HDL ↑
Typical Dose: 145 mg once daily
CV Benefit: FIELD trial - modest CV risk reduction in diabetics with high TG
Side Effects: Liver enzyme rise, creatinine ↑, gallstones
Atorvastatin (Statin)
Primary Target: LDL ↓
Typical Dose: 10-80 mg daily
CV Benefit: PROVE-IT, IMPROVE-IT - strong reduction in MI, stroke
Side Effects: Myalgia, liver enzyme rise
Ezetimibe
Primary Target: LDL ↓ (add-on)
Typical Dose: 10 mg daily
CV Benefit: IMPROVE-IT - added benefit when combined with statin
Side Effects: GI upset, rare liver issues
Icosapent Ethyl (Omega-3)
Primary Target: Triglycerides ↓
Typical Dose: 2 g twice daily
CV Benefit: REDUCE-IT - 25% CV event cut in high-risk TG >150 mg/dL
Side Effects: Fishy after-taste, mild GI upset
Niacin
Primary Target: HDL ↑, TG ↓
Typical Dose: 500-2000 mg daily
CV Benefit: ARBITER - no clear CV outcome benefit
Side Effects: Flushing, itching, liver toxicity
When doctors prescribe Tricor (Fenofibrate) a lipid‑modifying medication that primarily lowers triglycerides, patients often wonder how it stacks up against other choices. Below you’ll get a straight‑forward look at what Tricor does, which drugs or strategies can be used instead, and how to decide what fits your health goals.
Key Takeaways
- Tricor targets high triglycerides and modestly raises HDL; it’s not a first‑line therapy for LDL reduction.
- Statins remain the most proven class for lowering LDL and reducing heart‑attack risk.
- Ezetimibe and omega‑3 fatty acids can complement or replace Tricor in specific scenarios.
- Side‑effect profiles differ: Tricor may affect liver enzymes and kidney function, while statins can cause muscle aches and omega‑3s are generally gentle.
- Choosing the right regimen hinges on your lipid panel numbers, underlying conditions, and how you tolerate each drug.
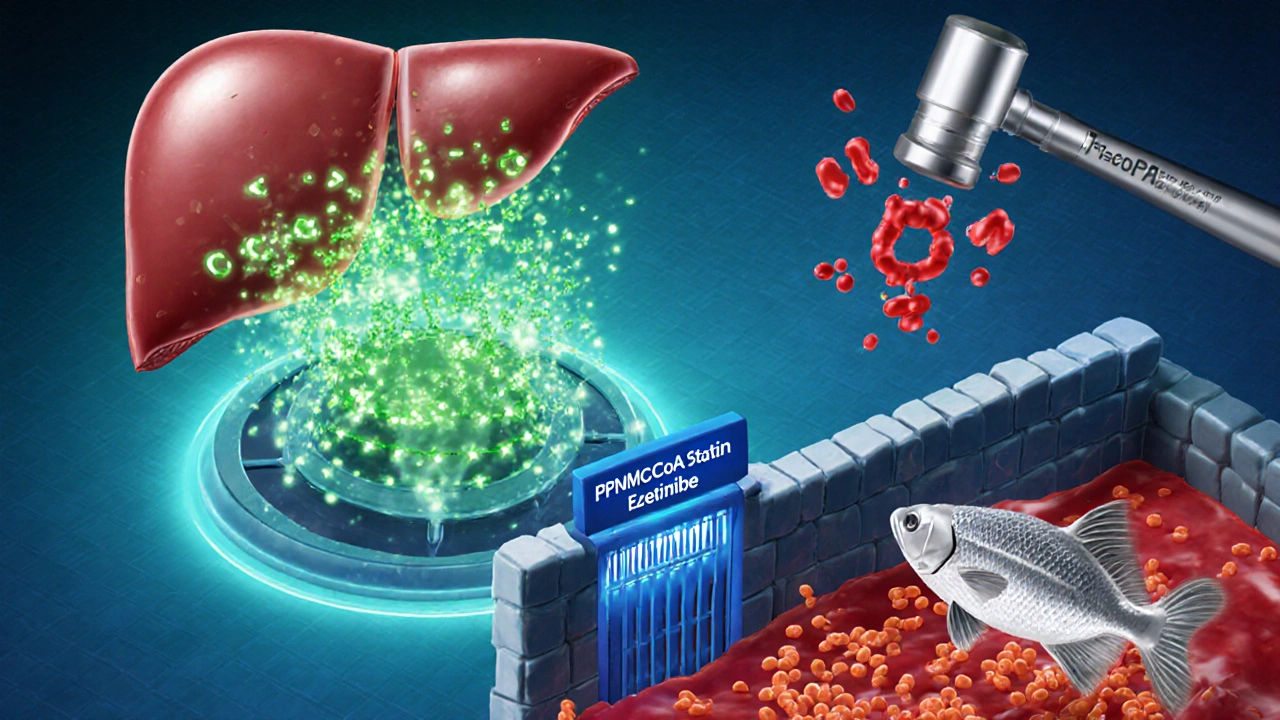
How Tricor Works
Fenofibrate belongs to the fibrate class. It activates the peroxisome proliferator‑activated receptor‑alpha (PPAR‑α), which ramps up the breakdown of fatty acids in the liver and muscles. The result is a 30-50% drop in triglycerides, a 10-20% rise in HDL‑C, and a modest (5-10%) reduction in LDL‑C. Because its main impact is on triglyceride metabolism, clinicians usually reserve Tricor for patients with:
- Triglyceride levels above 200mg/dL (2.3mmol/L) despite diet.
- Mixed dyslipidaemia where LDL is already at target.
- Risk of pancreatitis due to very high triglycerides.
Core Alternatives to Tricor
Several other options can lower lipids, each with a different focus.
Statins (e.g., Atorvastatin)
Statins inhibit HMG‑CoA reductase, the key enzyme for cholesterol synthesis. They are the gold standard for reducing LDL‑C (up to 60%) and have the strongest evidence for cutting heart‑attack and stroke rates.
Ezetimibe
Ezetimibe blocks intestinal absorption of cholesterol. When added to a statin, it can shave another 15-20% off LDL‑C, making it useful for patients who can’t tolerate high‑dose statins.
Omega‑3 Fatty Acids (e.g., Icosapent Ethyl)
Omega‑3 fatty acids reduce hepatic triglyceride production and have anti‑inflammatory effects. Prescription‑grade EPA (icosapent ethyl) can cut triglycerides by 30% and has shown cardiovascular benefit in high‑risk patients with elevated triglycerides.
Niacin (Nicotinic Acid)
Niacin raises HDL‑C and lowers triglycerides, but its use has fallen because of flushing, liver toxicity, and limited outcome data.
Lifestyle Changes
A diet low in refined carbs and saturated fats, regular aerobic exercise, weight loss, and limiting alcohol can lower triglycerides by 20-30% on their own. Lifestyle is always the foundation, even when drugs are added.
Side‑Effect Snapshot
Understanding tolerability helps narrow the field.
- Tricor: May increase liver enzymes, elevate serum creatinine, and cause gallstones in rare cases.
- Statins: Muscle aches (myopathy), rare rhabdomyolysis, slight rise in liver enzymes.
- Ezetimibe: Generally well‑tolerated; occasional digestive upset.
- Omega‑3s: Fishy after‑taste, mild GI upset; prescription forms have minimal bleeding risk.
- Niacin: Intense flushing, itching, potential liver strain.
Head‑to‑Head Comparison
| Medication | Primary Target | Typical Dose | Key Evidence for CV Benefit | Common Side Effects |
|---|---|---|---|---|
| Tricor (Fenofibrate) | Triglycerides ↓, HDL ↑ | 145mg once daily | FIELD trial - modest CV risk reduction in diabetics with high TG | Liver enzyme rise, creatinine ↑, gallstones |
| Atorvastatin (Statin) | LDL ↓ | 10‑80mg daily | PROVE‑IT, IMPROVE‑IT - strong reduction in MI, stroke | Myalgia, liver enzyme rise |
| Ezetimibe | LDL ↓ (add‑on) | 10mg daily | IMPROVE‑IT - added benefit when combined with statin | GI upset, rare liver issues |
| Icosapent Ethyl (Omega‑3) | Triglycerides ↓ | 2g twice daily | REDUCE‑IT - 25% CV event cut in high‑risk TG >150mg/dL | Fishy after‑taste, mild GI upset |
| Niacin | HDL ↑, TG ↓ | 500‑2000mg daily | ARBITER - no clear CV outcome benefit | Flushing, itching, liver toxicity |
When to Reach for Tricor
If your recent lipid panel shows:
- Triglycerides>200mg/dL (2.3mmol/L) and
- LDL already at goal (<100mg/dL for most) or you’re on a maximally tolerated statin,
then adding Tricor can bring triglycerides down quickly and improve HDL modestly. It’s especially useful for patients with metabolic syndrome or type‑2 diabetes who can’t achieve TG targets with diet alone.

When Alternatives Might Be Better
Consider these scenarios:
- High LDL, low TG: Statins (or a statin+ezetimibe combo) are first‑line.
- Very high TG (>500mg/dL): Prescription omega‑3s or high‑dose fibrates (including Tricor) are needed, but many clinicians start with omega‑3s because of better CV outcome data.
- Statin intolerance: Low‑dose rosuvastatin plus ezetimibe, or omega‑3s, can be alternatives.
- Desire to avoid pills: Lifestyle overhaul-Mediterranean diet, regular cardio, weight loss-can sometimes replace medication altogether.
Decision Checklist
- What lipid abnormality is most out of range?
- Are you already on a statin? If yes, at what dose?
- Do you have kidney or liver concerns that limit fibrate use?
- Is there a history of pancreatitis (very high TG) or cardiovascular events?
- How do you tolerate potential side effects (muscle pain vs. liver changes)?
Answering these questions guides you toward the drug that hits the right target with the fewest drawbacks.
Practical Tips for Taking Tricor
- Take the tablet with a full glass of water, preferably with food to ease stomach upset.
- Get baseline liver function tests and serum creatinine, then repeat after 6‑8 weeks.
- Avoid excessive alcohol, which can raise triglycerides and stress the liver.
- Stay hydrated; dehydration can increase the risk of kidney‑related side effects.
Frequently Asked Questions
Can I use Tricor together with a statin?
Yes. Combining a fibrate with a moderate‑intensity statin can address both high LDL and high triglycerides. Your doctor will monitor liver enzymes closely because the combo slightly raises the risk of liver issues.
Is Tricor safe for people with kidney disease?
Fibrates, including fenofibrate, can increase serum creatinine. In mild to moderate chronic kidney disease (eGFR>30mL/min) they’re often still used, but dosage may be reduced and labs checked more often.
How fast does Tricor lower triglycerides?
Most patients see a 20‑30% drop within 4‑6 weeks, with the full effect by 12 weeks.
Do I need to stay on Tricor for life?
If triglycerides stay low after diet, weight loss, and exercise, some doctors may taper off the drug. However, many patients with genetics‑driven hypertriglyceridemia stay on it indefinitely.
What’s the difference between prescription omega‑3s and fish‑oil supplements?
Prescription products contain purified EPA (or EPA+DHA) at doses proven to lower TG and cut CV events. Over‑the‑counter supplements vary in strength and purity, making outcomes unpredictable.





Tricor can help lower those stubborn triglycerides.
While the mechanistic rationale for fenofibrate is sound, the clinical evidence remains modest. The FIELD trial demonstrated only a slight reduction in cardiovascular events among diabetics with elevated triglycerides. Consequently, clinicians should reserve Tricor for patients with refractory hypertriglyceridaemia rather than employing it as a first‑line agent.
Great overview! It really helps to see the side‑effect profile laid out side by side. If you’re battling high TGs and your LDL is already on target, Tricor can be a useful tool. Just remember to pair it with diet tweaks and regular labs, and you’ll keep things balanced.
Thanks for the clear table-makes comparison painless. For anyone hesitant about adding another pill, start with lifestyle changes and re‑check labs in 8‑12 weeks. If triglycerides stay high, a low‑dose fibrate like Tricor is a reasonable next step, especially under physician supervision.
Fenofibrate works but watch liver enzyems its not for everyone
One must acknowledge that the pharmacodynamics of fenofibrate are well‑characterized. Nevertheless, the marginal benefit in low‑risk populations fails to justify routine use. A judicious clinician will weigh cost, benefit, and patient preference before prescribing.
Reading this feels like flipping through a colorful atlas of lipid‑lowering options. The way Tricor gently nudges triglycerides down is almost poetic, especially when paired with a Mediterranean diet. If your heart’s a garden, think of each medication as a different seed-pick the right one for the soil you have.
People think pharma just pushes pills but the truth is hidden in the data streams the big labs don’t want you to see you know the omega‑3 trials were funded by fish farms and the fibrates got quiet support from big agriculture that benefits from higher cholesterol markets
Honestly, the only time I’d pick Tricor is when diets fail and the numbers are scary.
That’s a fair point. It’s important to remember that medication isn’t a magic wand; combining it with consistent exercise and a balanced diet often yields the best outcomes. If you’re monitoring labs regularly, you can catch any side effects early.
Allow me to elaborate on why the conversation around fenofibrate often suffers from oversimplification.
First, the pathophysiology of hypertriglyceridaemia is multifactorial, encompassing genetics, diet, insulin resistance, and hepatic lipid handling.
Second, the FIELD trial, while valuable, enrolled a very specific cohort-diabetic patients with elevated triglycerides-limiting generalizability.
Third, subsequent meta‑analyses have shown that the absolute risk reduction in major adverse cardiovascular events is modest at best, hovering around 5‑7% in high‑risk subsets.
Fourth, the side‑effect profile, although generally tolerable, includes elevations in liver enzymes and creatinine, which necessitates periodic monitoring.
Fifth, the interplay with statins is not without concern; combined fibrate‑statin therapy raises the specter of myopathy, especially with gemfibrozil, though fenofibrate carries a lower risk.
Sixth, alternative therapies such as prescription EPA (icosapent ethyl) have demonstrated a more robust 25% relative risk reduction in the REDUCE‑IT trial for patients with similar triglyceride elevations.
Seventh, lifestyle modification remains the cornerstone-reducing simple carbohydrates, increasing omega‑3 intake through diet, and regular aerobic activity can lower triglycerides by 20‑30% without pharmacologic risk.
Eighth, patient adherence tends to be higher with once‑daily dosing, which favours Tricor’s simplicity compared to some multi‑dose regimens.
Ninth, cost considerations vary by region; generic fenofibrate is often affordable, whereas branded omega‑3 formulations can be expensive.
Tenth, clinicians must individualize therapy based on the dominant lipid abnormality: LDL‑centric patients benefit more from statins, whereas triglyceride‑centric patients may need a fibrate or EPA.
Eleventh, recent guidelines suggest reserving fibrates for triglycerides >200 mg/dL or when pancreatitis risk is present.
Twelfth, patient education about potential flushing, gastrointestinal upset, and the importance of periodic labs cannot be overstated.
Thirteenth, emerging research on PPAR‑α agonists hints at future agents with better efficacy and safety profiles.
Fourteenth, shared decision‑making empowers patients to weigh the modest CV benefit against the monitoring burden.
Fifteenth, in practice, many physicians opt for a stepwise approach: diet, then statin, then add either ezetimibe, omega‑3, or fenofibrate as needed.
Sixteenth, the bottom line is that fenofibrate remains a useful tool in a nuanced therapeutic arsenal, but it is not a universal solution.
Seventeenth, each patient’s comorbidities, preferences, and lab trends should guide the final choice.
Oh sure, because we all love popping pills like candy 🍬. If only the side‑effects were as sweet as the marketing hype.
I must disagree with that tone; the reality is far more nuanced than a sugary analogy. Dismissing the evidence with sarcasm undermines constructive dialogue.
The table does a solid job of laying out the options. It’s helpful for anyone trying to navigate the maze of lipid‑lowering meds.
Excellent work presenting the data-truly illuminates the path forward for patient care. I appreciate the thoroughness and clarity, even if a few tiny typos sneaked through. Let’s continue to champion evidence‑based choices for healthier hearts.
The content is balanced, though I’d caution against over‑reliance on any single agent without considering overall risk profile.
What a vibrant guide! It’s like a beacon of hope for anyone overwhelmed by cholesterol jargon. Keep the optimism flowing, because better health is truly within reach.
Thank you for the calm, friendly tone. It’s refreshing to see scientific discussion presented in a way that feels inclusive and approachable.