
radiation therapy eye cancer may sound like a high‑tech phrase, but it’s actually a life‑saving option for people diagnosed with tumors inside the eye. Whether you or a loved one are facing a new diagnosis, understanding how radiation works, what types are available, and what to expect can make the journey less daunting.
Key Takeaways
- Radiation therapy is a primary curative option for most primary eye cancers, especially uveal melanoma and retinoblastoma.
- Three main modalities are used: plaque brachytherapy, proton beam therapy, and external beam radiation therapy (EBRT).
- Vision‑preservation rates range from 60% to 80% depending on tumor size and treatment choice.
- Side‑effects are generally manageable and monitored through a structured follow‑up plan.
- Choosing the right technique involves tumor characteristics, patient age, and available expertise.
What Is Eye Cancer?
Eye cancer, medically referred to as ocular malignancy covers any malignant growth arising within the eye’s structures, most commonly in the uveal tract (uveal melanoma) or the retina (retinoblastoma). Uveal melanoma accounts for about 80% of adult eye cancers, while retinoblastoma is the leading intra‑ocular tumor in children. Both can threaten vision and, if untreated, spread beyond the eye.
Why Radiation Therapy?
Historically, surgery - enucleation (removal of the eye) - was the only cure for many ocular tumors. Advances in imaging and radiation delivery now allow clinicians to target the tumor precisely, preserving the globe and often maintaining useful sight. Radiation therapy acts directly on DNA, breaking the strands that cancer cells need to multiply, while modern techniques spare surrounding healthy tissue.
Types of Radiation Used in Eye Cancer
The choice of radiation depends on tumor size, location, and patient factors. Below are the three most common approaches, each with its own workflow and outcomes.
Plaque Brachytherapy
Plaque brachytherapy involves suturing a small, radiation‑seed‑filled disc (the plaque) directly onto the sclera over the tumor for several days. Radioactive isotopes such as iodine‑125 or ruthenium‑106 deliver a high dose locally, then the plaque is removed.
- Ideal for medium‑sized choroidal melanomas (3-10mm thickness).
- Procedure lasts 3-7 days, usually performed under local anesthesia.
- Vision preservation rates of 70% in tumors ≤5mm thick.
Proton Beam Therapy
Proton therapy uses a narrow beam of protons whose energy can be tuned to stop precisely at the tumor depth, minimizing exit dose. It’s particularly useful for large or irregularly shaped tumors located near critical structures like the optic nerve.
- Available at dedicated centers (e.g., Paul Scherrer Institute, Massachusetts General Hospital).
- Typical regimen: 4-5 fractions over one week.
- Reported 5‑year eye‑preservation rates up to 85% for large melanomas.
External Beam Radiation Therapy (EBRT)
External beam radiation therapy delivers high‑energy X‑rays or electrons from a machine outside the body, shaping the beam to match the tumor’s outline. Techniques such as intensity‑modulated radiation therapy (IMRT) or stereotactic radiosurgery (SRS) improve precision.
- Used when plaque placement is technically difficult (e.g., anterior tumors).
- Typical dose: 45-50Gy in 20-25 fractions.
- Eye‑preservation outcomes vary, generally 60-70% for small‑to‑medium lesions.
How Treatment Is Planned and Delivered
- Diagnostic Imaging: High‑resolution ultrasound, fundus photography, and MRI map the tumor’s exact dimensions.
- Tumor Board Review: A multidisciplinary team (ophthalmic oncologist, radiation physicist, medical physicist, retina specialist) decides the optimal modality.
- Simulation: For external beam and proton therapy, the patient lies on a custom‑made immobilization mask; CT simulation captures eye position. \n
- Treatment Planning: Specialized software creates a 3‑D dose distribution, aiming for a therapeutic dose (>80Gy) to the tumor while keeping the lens, optic nerve, and macula under tolerance levels.
- Delivery: Days to weeks of daily sessions (or a single high‑dose session for brachytherapy) are performed under close supervision.
- Post‑Treatment Imaging: A follow‑up scan confirms dose coverage and checks for early complications.

Benefits and Expected Outcomes
When executed by an experienced ophthalmic oncology team, radiation therapy can eradicate the tumor while preserving the globe in 80% of cases. Specific benefits include:
- Vision preservation: Many patients retain enough visual acuity to read, drive, and work.
- Cosmetic outcome: The eye remains in place, avoiding the psychological impact of enucleation.
- Low systemic toxicity: Unlike chemotherapy, radiation is localized, so there’s no widespread immune suppression.
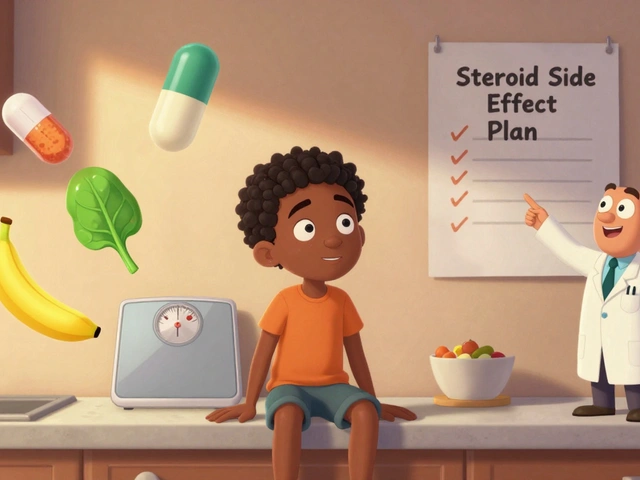
Risks and Side‑Effects
All radiation carries potential side‑effects, but modern delivery methods keep them manageable.
| Side‑Effect | Plaque Brachytherapy | Proton Therapy | EBRT |
|---|---|---|---|
| Radiation retinopathy | 5‑10% (often delayed 2‑5yr) | 2‑5% | 10‑15% |
| Dry eye / irritation | 15‑20% | 10‑12% | 20‑25% |
| Optic nerve damage | Rare (<2%) | 1‑3% | 3‑5% |
| Secondary cataract | Up to 30% (dose‑dependent) | 10‑15% | 25‑30% |
Regular monitoring with retinal exams and OCT scans catches issues early, allowing laser or anti‑VEGF injections to mitigate vision loss.
Choosing the Right Approach
Decision‑making hinges on a few key factors:
- Tumor size & location: Small, posterior lesions often fare best with plaque brachytherapy; large or anterior lesions may need proton or EBRT.
- Patient age: Children with retinoblastoma typically receive systemic chemotherapy plus focal laser, reserving radiation for refractory cases.
- Facility expertise: Access to a dedicated proton center can improve outcomes for complex tumors.
- Visual goals: If the tumor is near the macula, preserving central vision may guide modality choice.
Discuss these points openly with your ophthalmic oncologist - a personalized plan yields the best balance of cure and quality of life.
Aftercare and Follow‑Up
Post‑treatment care is essential for long‑term success.
- First‑Month Review: Dilated fundus exam to assess tumor regression and early side‑effects.
- Quarterly Checks (Year1): Visual acuity testing, OCT imaging, and fluorescein angiography as needed.
- Annual Surveillance (Years2‑5): Detect late radiation retinopathy or secondary malignancies.
- Lifelong Monitoring: Even after five years, some centers recommend a yearly exam because late complications can appear.
Most patients resume normal activities within a week of plaque removal or a few days after external beam sessions. Maintaining eye‑health habits - protective sunglasses, control of systemic hypertension, and prompt reporting of visual changes - supports optimal recovery.
Frequently Asked Questions
What is plaque brachytherapy and how is it performed?
A tiny gold disc, called a plaque, is sutured to the sclera over the tumor. Radioactive seeds inside the plaque emit radiation for a set number of days (usually 3-7). After the dose is delivered, the plaque is removed. The whole procedure is done under local anesthesia and takes a few hours.
Who is a good candidate for proton therapy?
Patients with large (>10mm) or irregularly shaped uveal melanomas, tumors close to the optic nerve, or those who cannot undergo plaque surgery are typical candidates. Access to a proton center is required.
How long does radiation treatment take?
Plaque brachytherapy lasts 3-7 days of in‑eye placement. Proton therapy is usually completed in 4-5 sessions over one week. External beam regimens can span 3-5 weeks, with daily fractions.
Will radiation therapy affect my vision permanently?
Most patients retain usable vision, especially when the tumor is not centered on the macula. Some may develop cataracts, dry eye, or radiation retinopathy, which can often be treated. Regular follow‑up helps catch and manage these changes early.
Is radiation therapy safe for children with retinoblastoma?
Radiation is used sparingly in children because of the risk of secondary cancers. It’s reserved for tumors that don’t respond to chemotherapy or laser. When needed, proton therapy is preferred due to its precise targeting.




Radiation therapy represents a profound shift in the management of ocular malignancies, allowing clinicians to target neoplastic tissue while preserving the integrity of the globe. By delivering ionizing energy with precision, modalities such as plaque brachytherapy, proton beam, and external beam techniques mitigate the need for enucleation in many cases. The preservation of visual function, even when partial, profoundly impacts patient quality of life, especially for those whose professions depend on sight. Moreover, multidisciplinary tumor boards ensure that the chosen modality aligns with tumor dimensions, anatomical considerations, and patient comorbidities. It is essential to appreciate that the therapeutic window balances maximal tumoricidal effect against the tolerance thresholds of delicate ocular structures. Consequently, informed consent must encompass not only efficacy statistics but also the nuanced spectrum of potential sequelae.
The dosimetric planning algorithm employs three‑dimensional conformal mapping to achieve a conformity index exceeding 0.9, thereby optimizing the biologically effective dose to the choroidal mass while preserving the optic nerve’s dose–volume histogram constraints. Isodose curves are sculpted using inverse planning software, integrating Monte Carlo simulations to account for heterogeneities in ocular tissue density. Additionally, the linear-quadratic model guides fractionation schemes, ensuring an α/β ratio appropriate for melanocytic proliferation. These technical nuances substantiate the reported 80 % globe‑preservation statistics.
That’s good to hear – radiation can really save an eye without taking it out. The procedures aren’t as scary as they sound, and most docs walk you through every step. You’ll get regular check‑ups to catch any side‑effects early. Stay positive and keep talking with your care team.
Honestly this whole “radiation saves eyes” hype is overblown it’s just another dangerous gamble
Wow, the variety of options is amazing! From tiny plaques perched on the sclera to high‑tech proton beams, the field feels like something out of a sci‑fi movie. It’s comforting to know that preserving vision isn’t a pipe dream any more. The multidisciplinary approach truly puts the patient at the centre of care. Keep spreading the word – knowledge is power!
Sure, because everyone’s just lounging around waiting for a proton beam like it’s a coffee shop latte.
It must be emphasized, therefore, that the implementation of plaque brachytherapy, indeed, necessitates meticulous surgical asepsis, precise isotopic calibration, and a postoperative regimen comprising serial fundoscopic examinations; similarly, proton beam therapy requires, without exception, access to a cyclotron‑based facility, interdisciplinary coordination, and stringent quality‑assurance protocols; finally, external beam radiation, while more widely available, obliges the practitioner to employ intensity‑modulated techniques, safeguard the macular region, and monitor for radiation‑induced retinopathy with diligent follow‑up.
All that “precision” is a cover‑up for Big Pharma pushing cheap tech while the real cure is hidden
Radiation therapy for eye cancer isn’t just a medical procedure, it’s a journey that reshapes a patient’s future. First, the diagnosis itself can feel like a dark cloud hanging over everyday life, but the availability of targeted treatments offers a silver lining. When a plaque is sutured onto the sclera, it might sound intimidating, yet the procedure is done under local anaesthesia and the patient can often go home the same day. The isotopes inside the plaque emit radiation that bathe the tumor in a controlled dose, sparing the surrounding retina. Over the next few days, the radiation works at the cellular level, breaking DNA strands of malignant cells while leaving healthy tissue largely untouched. After removal of the plaque, the eye begins a healing process that is closely monitored by a team of specialists. Regular ultrasounds and fundus photographs track the tumor’s response, providing reassurance that the treatment is effective. If the tumor was large or irregular, proton beam therapy may be chosen; its pinpoint accuracy means the beam stops right at the tumour’s depth, virtually eliminating exit dose. This can be a lifesaver for lesions near the optic nerve where conventional methods risk vision loss. External beam radiation, although more common, still benefits from modern intensity‑modulated techniques that shape the dose to the tumor’s contours. Side‑effects, such as dry eye or cataract formation, are potential, but they are manageable with drops, lenses, or surgery down the line. Importantly, preserving the eye itself carries profound psychological benefits – the patient retains a familiar appearance and avoids the trauma of enucleation. Studies have shown that 60‑80 % of patients maintain usable vision, allowing them to read, drive, or enjoy hobbies they love. The interdisciplinary tumor board, composed of oncologists, ophthalmologists, physicists, and nurses, collaborates to tailor the optimal regimen for each individual case. Such collaboration ensures that decisions are evidence‑based and patient‑centered. Ultimately, the success of radiation therapy lies not only in eradicating cancer but also in restoring hope and normalcy to those affected.
Yo the long post is cool but u gotta remember that the LQ model and BED calculations are the real game changers – without proper RBE accounting you’re just guessin