
Return-to-Play Readiness Checker
This tool helps athletes assess their readiness to return to play based on their current rehabilitation progress.
Injury Details
Readiness Assessment
Estimated Time Until Full Return:
Recovery Progress: %
When you’re sidelined by a sports injury is a disruption that feels personal. The good news is that a structured Return-to-Play Rehabilitation a step‑by‑step program that helps athletes regain function while minimizing re‑injury risk can get you back on the field safely.
- Pinpoint the injury’s current status before you start any training.
- Work with a qualified physical therapist to design a personalized plan.
- Focus on strength, flexibility, and neuromuscular control in that order.
- Follow a clear, phased return‑to‑play protocol, adjusting as needed.
- Watch for warning signs and never push through pain.
Step 1: Assess the Injury
Before you lace up your shoes, you need a realistic picture of where you stand. A thorough assessment includes:
- Medical imaging (MRI, X‑ray) if recommended.
- Range‑of‑motion testing performed by a qualified professional.
- Strength comparison between the injured and uninjured side.
- Functional tests that mimic sport‑specific movements.
These data points help your physical therapist set realistic milestones and avoid rushing the process.
Step 2: Get Professional Guidance
Self‑managed rehab can work for minor bruises, but most sports injuries benefit from a specialist. A physical therapist brings three key skills:
- Diagnosis refinement - they can spot subtle deficits that indicate underlying issues.
- Exercise prescription - they match load, speed, and volume to your recovery stage.
- Progress monitoring - they use objective criteria (e.g., hop test distance) to confirm readiness for the next phase.
Make sure your therapist holds appropriate credentials (e.g., PT, DPT) and has experience with your sport.
Step 3: Design the Rehabilitation Plan
Think of rehabilitation as a layered puzzle. Each piece builds on the previous one, ensuring the body adapts without overload.
Typical phases include:
- Acute management - control inflammation, protect tissues, gentle mobility.
- Restoration - regain full range of motion and begin low‑load strength work.
- Optimization - increase load, add sport‑specific drills, improve neuromuscular control.
- Maintenance - transition to full training while monitoring fatigue.
Each phase lasts anywhere from a few days to several weeks, depending on the injury’s severity and your baseline fitness.
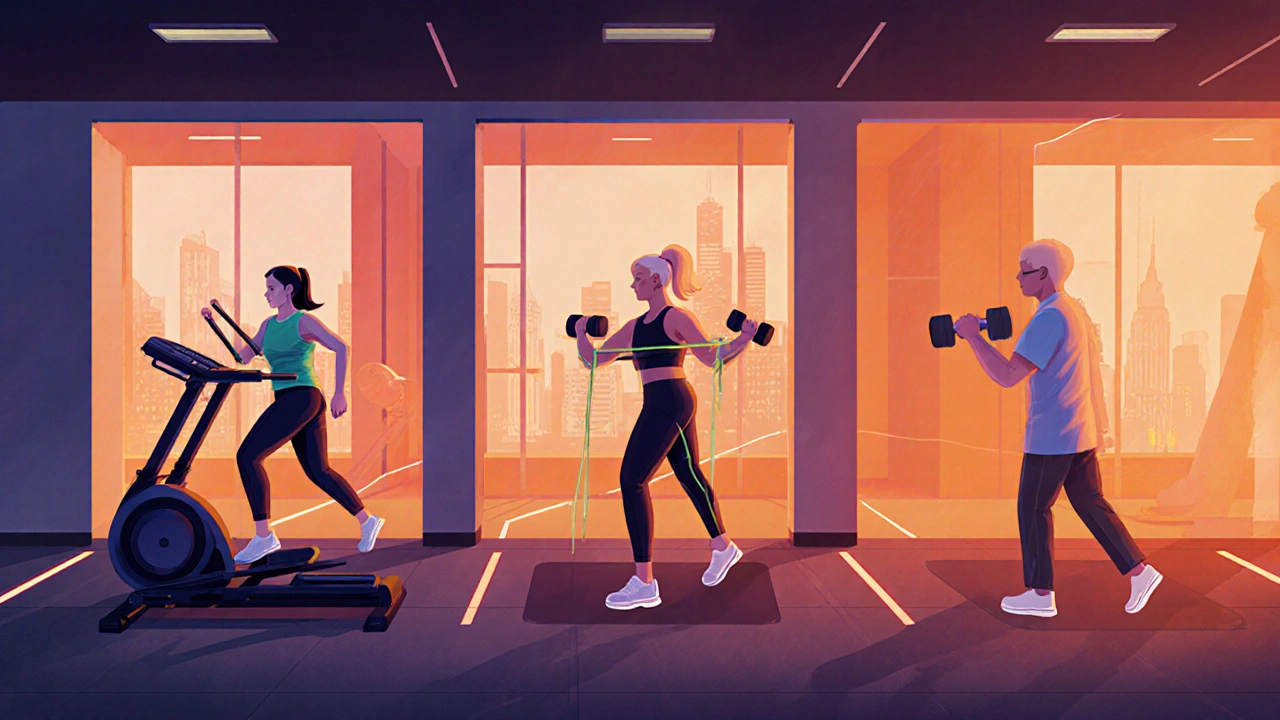
Step 4: Prioritize Strength and Flexibility
Two pillars keep you from re‑injuring: strength training and flexibility exercises. Here’s how to blend them effectively.
Strength Training
Start with closed‑chain movements (e.g., squats, lunges) that mimic real sports patterns. Progress to single‑leg or unilateral drills once bilateral strength is solid. Aim for 2‑3 sessions per week, focusing on:
- Core stability - planks, dead‑bugs, pallof presses.
- Hip and knee control - side‑step bands, terminal knee extensions.
- Upper‑body power - push‑ups, medicine‑ball throws.
Flexibility Exercises
Dynamic stretching before workouts prepares muscles for speed, while static stretching after sessions restores length. Incorporate proprioceptive neuromuscular facilitation (PNF) holds for the most stubborn tight spots.
Step 5: Follow a Structured Return‑to‑Play Protocol
The heart of a safe comeback is a phased protocol that matches load to tissue healing. Below is a commonly used 5‑phase model. Adjust the time frames based on your therapist’s assessment.
| Phase | Typical Duration | Primary Goal | Key Activities |
|---|---|---|---|
| Phase 1 - Protection | 1‑2 weeks | Control pain & swelling | Ice, compression, gentle ROM |
| Phase 2 - Activation | 2‑4 weeks | Restore mobility & basic strength | Isometric holds, low‑load bands |
| Phase 3 - Load Progression | 4‑8 weeks | Build sport‑specific endurance | Interval runs, plyometrics, weighted drills |
| Phase 4 - Skill Integration | 8‑12 weeks | Re‑introduce technical skills | Cutting drills, jump‑landing, position drills |
| Phase 5 - Full Competition | 12+ weeks | Achieve pre‑injury performance | Full‑strength scrimmages, game‑speed reps |
Progress to the next phase only when you meet objective criteria (e.g., pain‑free single‑leg hop, <10% asymmetry on strength tests).
Step 6: Watch for Warning Signs
Even with a perfect plan, the body can send red flags. Keep an eye on:
- Sharp or lingering pain that worsens with activity.
- Swelling that appears during or after a session.
- Loss of coordination or a feeling of “giving way”.
- Excessive fatigue that doesn’t improve with rest.
If any of these pop up, pause the program and consult your therapist. Ignoring them often leads to chronic issues.
Step 7: Use Protective Equipment and Optimize the Environment
Sometimes a simple gear change makes a huge difference. Consider:
- Bracing - a well‑fitted knee or ankle brace can limit harmful motions during early return phases.
- Footwear - choose shoes that provide appropriate cushioning and lateral support for your sport.
- Playing surface - softer turf or grass reduces impact forces compared to hard courts.
These tools are not a substitute for strength, but they add a safety net while you rebuild confidence.
Step 8: Train Your Mind
Physical readiness is only half the battle. Mental readiness-focus, confidence, and managing fear-keeps you from sabotaging progress. Simple strategies:
- Visualization: picture yourself executing a skill flawlessly.
- Goal‑setting: break the protocol into weekly, achievable targets.
- Mindfulness breathing: lowers anxiety before high‑intensity drills.
If anxiety spikes, talk to a sports psychologist or a trusted coach. A calm mind speeds up physical healing.
Putting It All Together
Returning to sport safely isn’t a mystery; it’s a systematic process. Start with a clear injury assessment, enlist a qualified physical therapist, and follow a phased return-to-play protocol. Combine strength, flexibility, protective gear, and mental strategies, and you’ll reduce the risk of setbacks.
When you hit that first game‑day after a long break, the goal isn’t just to play - it’s to play smarter and stronger.

Frequently Asked Questions
How long does a typical sports injury rehab take?
Recovery time varies widely. Minor strains may heal in 2‑4 weeks, while ligament repairs can require 3‑6 months. The key is progressing based on objective criteria, not a calendar.
Can I do any exercises on my own before seeing a therapist?
Gentle range‑of‑motion work and low‑impact cardio (like stationary biking) are generally safe. Avoid resistance or plyometric moves until a professional evaluates the tissue’s capacity.
What’s the biggest mistake athletes make during rehab?
Rushing the load. Athletes often think “I was good before, so I should be back now.” Skipping phases or ignoring pain leads to re‑injury and longer downtime.
Should I wear a brace throughout the whole rehab?
Use a brace only during the early load‑progression phases when the joint is still regaining stability. Once strength and proprioception are restored, taper off the brace to avoid dependence.
How can I tell if I’m ready for full competition?
You should meet three objective markers: (1) No pain during sport‑specific drills, (2) Less than 10% strength asymmetry between limbs, and (3) Ability to complete a full‑intensity practice without excessive fatigue.





Getting back on the field after an injury can feel scary, but a solid plan makes all the difference. Start by honestly rating your pain, mobility, and strength-those numbers guide every next step. Celebrate tiny wins like a pain‑free squat or a smoother hop; they’re real signs you’re progressing. Remember, the rehab phases aren’t just boxes to tick, they’re building blocks for confidence. Keep the momentum, stay patient, and you’ll soon be back doing what you love!
While the enthusiasm is commendable, the outlined protocol omits several evidence‑based considerations. For instance, the emphasis on static stretching post‑exercise disregards recent findings favoring dynamic mobility drills. Moreover, the pain threshold of three on a ten‑point scale is overly simplistic and fails to account for individual variability. A more nuanced assessment, perhaps integrating the Lower Extremity Functional Scale, would enhance clinical relevance. In its current form, the guide risks encouraging premature return‑to‑play.
Oh boy, here we go again with the textbook mumbo‑jumbo! You can feel the tension building like a storm before the match, and suddenly everyone’s a critic. The rehab plan sounds solid on paper, but real athletes need that gritty, gut‑feel edge. If you’re not sweating through the pain, are you even trying? Bottom line: keep the science, but don’t let it smother the fire.
Listen, folks-most of this “return‑to‑play” nonsense is just a fancy excuse for coaches to keep control. They’ll push you through pain because they want you on the roster, not because they care about your health. In America we’re taught to push through, but that’s a cultural myth that does more harm than good. If you want a real recovery, ditch the hype and listen to your own body, not the playbook. Anything else is just corporate agenda masquerading as science.
I hear the frustration, and I’m sorry you’ve felt that pressure. It’s true that some programs can feel like they’re driven by a win‑at‑all‑costs mentality. Yet many physical therapists genuinely prioritize long‑term health over short‑term glory. By collaborating with someone you trust, you can tailor the phases to respect your limits while still making progress. Remember, healing isn’t a race; it’s a journey that deserves patience and compassion.
The so‑called “phased protocol” is just a marketing gimmick.
First, let me say that the checklist looks promising but it’s only as good as the athlete’s honesty. If you fudge the pain score, the whole algorithm collapses. Second, the progression percentages feel arbitrary; I’d rather see a criterion based on functional testing. Third, mobility and strength should be measured with reliable tools, not just a 0‑10 guess. Fourth, the time estimates ignore individual healing rates, genetics, and previous injuries. Fifth, you must incorporate neuromuscular control drills before moving to plyometrics. Sixth, the “Phase 4 – Skill Integration” should include sport‑specific decision making drills. Seventh, always reassess after each session, because a single bad day can set you back. Eighth, nutrition and sleep play a massive role; omitting them is a glaring oversight. Ninth, mental readiness is crucial; confidence can be the difference between a safe return and a re‑injury. Tenth, you should have a clear cut‑off pain threshold, but also consider swelling and stiffness. Eleventh, communication with the coach ensures training loads are adjusted appropriately. Twelfth, using video analysis can catch subtle gait asymmetries that the checklist misses. Thirteenth, don’t forget to warm‑up dynamically before every rehab session. Fourteenth, gradually re‑introduce competition drills under supervision. Fifteenth, celebrate the milestones, but stay vigilant because the risk never fully disappears.
One could argue that the checklist’s rigidity masks deeper philosophical questions about the nature of recovery; is healing merely a series of metrics or a holistic rebirth of the athlete’s identity? While the practical steps are useful, the omission of existential reflection may deprive the individual of true resilience. Moreover, the reliance on quantification echoes a mechanistic worldview that neglects the subtle interplay of mind, body, and spirit. In this sense, the protocol could benefit from integrating mindfulness practices to foster inner balance alongside physical metrics. Ultimately, without addressing the unseen dimensions, the program risks treating the body as a machine rather than a sentient being.
i dont buy that deep philosophical crap it’s just a rehab plan ignore the hype
Great discussion, everyone! Remember, the key to a safe comeback is listening to your body, sticking to the phased plan, and staying positive. Your therapist will help you fine‑tune each step, so trust the process and keep that fire alive. You’ve got this!