
Antihistamine Comparison Tool
Your Allergy Profile
Your Results
For millions of people with seasonal allergies, hay fever, or chronic hives, the old-school antihistamine routine used to be simple: take something like Benadryl, feel drowsy for hours, and hope it clears up the sneezing and itching. But if you’ve ever nodded off at your desk after taking diphenhydramine, you know why things changed. Today, most doctors and patients reach for second-generation antihistamines - drugs like loratadine, cetirizine, and fexofenadine - because they work just as well for allergies without knocking you out.
Why Second-Generation Antihistamines Are Different
First-generation antihistamines like diphenhydramine and chlorpheniramine were designed to block histamine, the chemical your body releases during an allergic reaction. But they didn’t stop there. These older drugs easily crossed the blood-brain barrier, messing with brain receptors and causing drowsiness, dry mouth, blurred vision, and even confusion in older adults. That’s why you couldn’t drive after taking them - and why they’re no longer the go-to for daily allergy relief. Second-generation antihistamines were built differently. Their molecules are larger and more polar, making it harder for them to slip into the brain. As a result, they target histamine receptors in your nose, skin, and throat - where allergies cause trouble - without affecting your central nervous system. Studies show they’re 72-89% less likely to cause drowsiness than first-gen options. Clinical trials report sedation rates of only 6-14% with second-gen drugs, compared to 50-60% with older ones.How They Work: More Than Just Blocking Histamine
It’s not just about staying awake. Modern research using cryo-electron microscopy has revealed exactly how these drugs bind to the H1 receptor. They latch onto a deep pocket in the receptor, locking it in place so histamine can’t trigger the allergic response. One 2024 study in Nature Communications even found a second binding site on the receptor, opening the door to even more precise future drugs. These medications are also longer-lasting. While first-gen antihistamines wear off in 4-6 hours, second-gen ones last 12 to 24 hours. That means one pill a day - no need to remember a midday dose. Peak levels hit your bloodstream in 1-3 hours, and they stay active long enough to cover your whole day, whether you’re at work, school, or outside gardening.The Top Three: Loratadine, Cetirizine, Fexofenadine
Not all second-generation antihistamines are the same. Here’s how the big three stack up:| Medication | Brand Name | Dose | Half-Life | Metabolism | Key Notes |
|---|---|---|---|---|---|
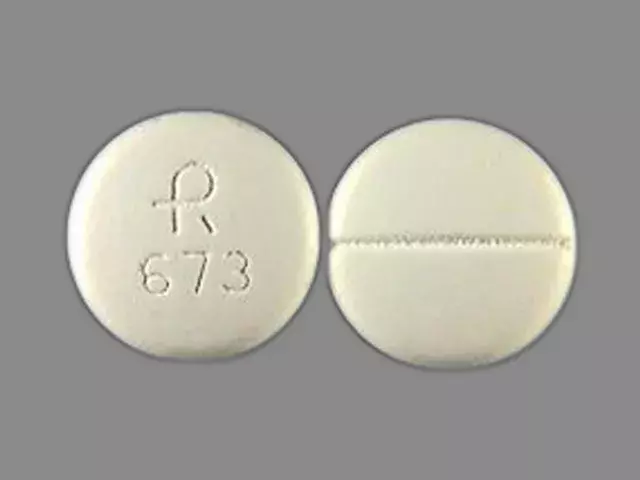
| Loratadine | Claritin | 10 mg daily | 8-18 hours | Mainly CYP3A4 | Lowest sedation risk, but some users report headaches |
| Cetirizine | Zyrtec | 10 mg daily | 8.3 hours | CYP3A4 and CYP2D6 | Most effective for itching; 23% of users report mild drowsiness |
| Fexofenadine | Allegra | 180 mg daily | 11-15 hours | Minimal metabolism; mostly excreted unchanged | Least likely to interact with other meds; safe with grapefruit juice |
Each has its strengths. Cetirizine is often the most effective for itching and hives, but it’s also the one most likely to cause mild sleepiness - even though it’s still far less than Benadryl. Loratadine is the gentlest on the nervous system, but some people swear it doesn’t work as well for them. Fexofenadine sits in the middle: reliable, with almost no drug interactions and no effect from grapefruit juice, which can interfere with other antihistamines.
What They Don’t Do - And Why You Might Still Feel Blocked Up
Here’s the catch: second-generation antihistamines are great for sneezing, runny nose, itchy eyes, and hives. But they don’t help much with nasal congestion. That’s because congestion comes from swollen blood vessels, not histamine. First-gen antihistamines had extra anticholinergic effects that could reduce mucus and swelling - but they also caused dry mouth and urinary retention. That’s why so many people end up using a nasal spray like Flonase or a decongestant like pseudoephedrine alongside their antihistamine. A 2023 Consumer Reports survey found that 41% of users needed extra meds just to feel fully relieved. If you’re still stuffed up after taking fexofenadine, it’s not you - it’s the drug’s limitation.Side Effects: Not Perfect, But Much Better
No drug is side-effect free. Even second-generation antihistamines can cause headaches, dry mouth, or nausea in a small number of people. Reddit users in r/Allergies report occasional taste disturbances - a weird metallic or bitter taste - especially with cetirizine. One user on Drugs.com said loratadine gave them three straight days of severe headaches until they switched to Zyrtec. Serious side effects are rare. The old second-gen drugs, terfenadine and astemizole, were pulled from the market in the late 90s because they caused dangerous heart rhythm changes when mixed with certain antibiotics or antifungals. But the current options - loratadine, cetirizine, and fexofenadine - have been closely monitored since then. The FDA’s post-marketing data through 2023 shows no significant cardiac risk with normal use. Fexofenadine, in particular, has almost no liver metabolism, making it the safest choice if you’re on other medications.Real People, Real Results
User feedback tells the real story. On WebMD, cetirizine has a 4.2 out of 5 rating from over 12,000 reviews. Most people say it works great - 78% call it “excellent” or “good.” But 23% still feel a little sleepy, which is higher than clinical trials suggest. Why? Maybe because real life isn’t a controlled study. People take it with meals, skip doses, or combine it with alcohol or other meds. One top-rated comment on Reddit sums it up: “Fexofenadine works great for my seasonal allergies without making me sleepy like Benadryl did, but I still need Flonase for congestion.” That’s the pattern: effective, non-sedating, but incomplete without a nasal spray.





Been on cetirizine for years and honestly? It’s a game-changer. No more afternoon naps after lunch, just clean air and zero brain fog. I used to hate spring until I switched.
Oh, so now we’re romanticizing pharmaceuticals as if they’re poetry? The H1 receptor isn’t a Shakespearean sonnet-it’s a biological lock, and we’re just fumbling with keys we don’t fully understand. How quaint that we call this ‘science’ when we’re still guessing at half the mechanisms. And yet, we trust it with our children’s nasal passages. How very modern of us.
lol i took fexofenadine for 3 days and my tongue felt like i licked a battery. also why is everyone actin like this is new? my grandma took benadryl in the 70s and lived to 94. also grapefruit juice? bro i drink it every morning and i’m fine. stop overcomplicating shit.
If you’re still using antihistamines at all, you’re doing it wrong. The real solution is avoiding allergens entirely. Stop letting your body be a chemical experiment. Clean your house. Use a HEPA filter. Wear a mask. Stop relying on drugs to fix laziness.
Wait so cetirizine gives you drowsiness? bro that’s just because you take it with dinner. take it in the morning on an empty stomach and you’ll be fine. also fexofenadine is overrated-loratadine is cheaper and works just as good. stop falling for brand names. also i’ve been taking it for 12 years and never had a headache. you’re probably just dehydrated.
The evolution of antihistamines reflects a broader paradigm shift in pharmacology-from blunt, systemic interventions to precision molecular targeting. The fact that we can now design molecules that selectively occupy peripheral H1 receptors while avoiding CNS penetration speaks to the sophistication of modern medicinal chemistry. This isn’t merely an improvement in tolerability; it’s a philosophical reorientation of therapeutic intent: to alleviate suffering without compromising consciousness. The 2024 Nature Communications paper revealing the secondary binding site on the H1 receptor is not just a discovery-it’s a herald of a new era in receptor pharmacology, where allosteric modulation may render sedation an artifact of outdated molecular design.
Yet, we persist in treating these medications as interchangeable commodities, ignoring individual metabolic variance. CYP3A4 polymorphisms can turn a ‘non-sedating’ agent into a soporific for some. And we wonder why clinical trial data diverges from real-world outcomes? Because we treat patients as data points, not as complex, genetically distinct organisms. The 23% sedation rate with cetirizine? That’s not a flaw in the drug-it’s a flaw in our assumption of uniformity.
And let us not forget the ecological dimension: rising pollen counts, driven by anthropogenic climate change, are not merely increasing symptom burden-they are accelerating pharmacological dependency. By 2050, we may need not just daily doses, but sustained-release formulations, or perhaps even gene-editing approaches to modulate mast cell reactivity. We are not merely treating allergies-we are managing the consequences of planetary degradation. And yet, our discourse remains trapped in the binary of ‘this pill vs that pill.’
Perhaps the true revolution isn’t in the drug, but in our willingness to see beyond the pill bottle-to recognize that health is not a pharmacological fix, but an ecological and systemic equilibrium we have disrupted. We need more than antihistamines. We need humility.
Thank you for this thorough breakdown. As a clinician, I’ve seen too many patients continue on first-gen antihistamines because they didn’t know alternatives existed. The key point you made about timing-taking the medication prophylactically-is critical. I now recommend patients start one week before peak pollen season. Also, I emphasize that fexofenadine’s lack of CYP metabolism makes it ideal for polypharmacy patients, especially the elderly on statins or antifungals. One note: the FDA’s label clarity score of 6.4/10 is unacceptable. We need standardized, plain-language labeling for OTC meds. Patients shouldn’t need a pharmacy degree to understand their own treatment.
Let’s be real-this whole ‘non-sedating’ thing is a marketing myth. Cetirizine? That’s just Benadryl with a PhD. The ‘molecular polarity’ argument? Cute. But I’ve had patients pass out at their desks on fexofenadine. And don’t get me started on the ‘no grapefruit interaction’ claim-when you’re on ketoconazole or verapamil, you’re still playing Russian roulette. This isn’t science, it’s corporate theater. They pulled terfenadine because it killed people, then slapped ‘new and improved’ on the next one and called it a win. We’re not curing allergies-we’re just making them less inconvenient while pretending we’ve solved something fundamental.
And the ‘second binding site’? That’s not a breakthrough-it’s a footnote. We’ve known about allosteric sites since the 80s. What we need is a drug that doesn’t just block histamine, but resets the immune system’s overreaction. That’s the real frontier. Not another pill that makes you slightly less sleepy.
The data presented is largely accurate, though the conflation of sedation rates between clinical trials and real-world usage requires contextual clarification. The 23% sedation rate with cetirizine in WebMD reviews likely reflects concurrent alcohol use, sleep deprivation, or concomitant CYP2D6 inhibitors-factors absent in controlled trials. Furthermore, the assertion that loratadine is ‘less effective’ for some is not evidence of inferior pharmacology, but rather individual pharmacokinetic variability. I recommend therapeutic trial periods of at least seven days with each agent before concluding efficacy. The FDA’s label clarity score, while concerning, is a regulatory failure, not a pharmacological one.
bro i tried all three and zyrtec made me feel like i was underwater. loratadine did nothing. fexofenadine? kinda worked but i still needed sudafed. also why is everyone acting like this is deep? it’s just medicine. i just want to stop sneezing. also i think we should all just move to the desert.
To anyone still on Benadryl: you’re not weak. You’re just trying to survive. Many of us didn’t have access to these meds until recently-or we were told they were ‘too expensive.’ I’m so glad this post exists because it normalizes the struggle. I’ve been on fexofenadine for three years, and yes, I still need Flonase. That’s okay. You don’t need to be a superhero to manage allergies. You just need the right tools. And if one drug doesn’t work? Try another. It’s not failure-it’s fine-tuning. You’re not broken. You’re just allergic.
This whole post reads like a pharmaceutical ad. ‘Second-generation’ sounds fancy but it’s just repackaged old drugs with a higher price tag. The fact that 41% still need nasal sprays proves these aren’t solutions-they’re compromises. And the ‘real people’ quotes? All cherry-picked. Where are the people who got worse? Where’s the data on long-term immune suppression? You’re selling hope, not science.
I remember the days when my eyes would swell shut and I’d have to call in sick every April. I tried everything-neti pots, nasal rinses, even acupuncture. Nothing worked like cetirizine. But here’s the thing: it didn’t work the first time I took it. I thought it was useless. Then I read the fine print: ‘take daily for best results.’ So I did. For three weeks straight. And then one morning, I woke up and realized I hadn’t sneezed once. It wasn’t magic. It was consistency. If you’re giving up after two days, you’re not giving the medicine a chance-you’re giving up on yourself. And if you’re still congested? Add the spray. Don’t shame yourself for needing help. Your body isn’t broken. It’s just allergic. And you’re allowed to use tools to live well.