Essential Generics: What They Are, Why They Work, and How to Use Them Safely
When you hear essential generics, affordable versions of brand-name medications that meet the same strict standards for safety and effectiveness. Also known as generic medications, they make up over 90% of prescriptions filled in the U.S. because they save patients billions every year without cutting corners on quality. These aren’t cheap knockoffs—they’re exact copies in active ingredients, dosage, and how they work in your body. The FDA requires them to be bioequivalent, meaning they deliver the same results as the original drug, whether it’s your blood pressure pill, thyroid med, or antibiotic.
Behind every generic drug, a medication approved by the FDA as therapeutically equivalent to a brand-name drug is a complex system of testing, manufacturing, and oversight. The FDA inspection, a rigorous review of manufacturing facilities to ensure compliance with current Good Manufacturing Practices process checks everything from raw materials to packaging. If a plant fails, the FDA can block production until it fixes the issue. That’s why you can trust a generic from a reputable pharmacy—even if it costs 80% less. And it’s not just about price. The generic drug approval, the process by which the FDA reviews and authorizes a generic version of a brand-name drug for sale system, powered by user fees under GDUFA, cuts approval times from years to months. That means new generics hit the market faster, driving competition and lowering prices even more.
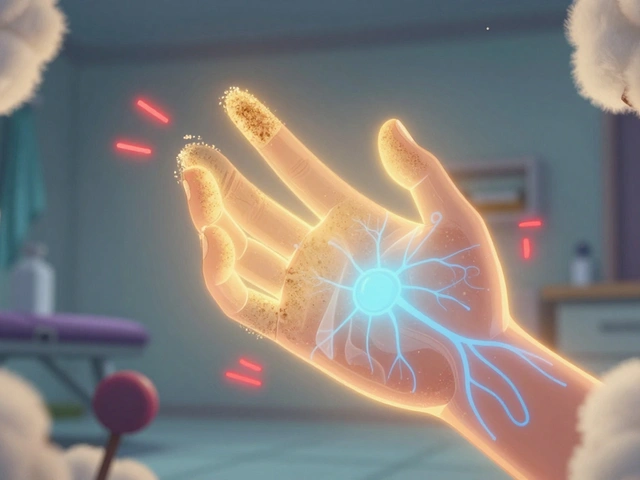
But not all generics are created equal in perception. Some people worry they’re less effective, or that switching from brand to generic causes problems. The truth? For the vast majority of drugs, there’s no difference in how they work. Studies show patients do just as well on generics for conditions like high blood pressure, diabetes, and depression. What does matter is consistency—sticking with the same generic manufacturer when possible, especially for drugs with narrow therapeutic windows like warfarin or levothyroxine. And always check your label. If your pill looks different, ask your pharmacist why. That’s not a red flag—it’s normal. But if you notice side effects you didn’t have before, speak up. Your body might be reacting to an inactive ingredient, not the medicine itself.
What you’ll find below is a curated collection of real, practical guides on how essential generics fit into your health. From how the FDA ensures they’re safe, to why soy can interfere with thyroid meds, to how genetic differences affect how your body handles them—these aren’t theoretical discussions. They’re based on real patient experiences, clinical data, and regulatory insights. Whether you’re trying to save money, manage a chronic condition, or just want to understand what’s in your medicine cabinet, this is the no-fluff, straight-to-the-point resource you need.