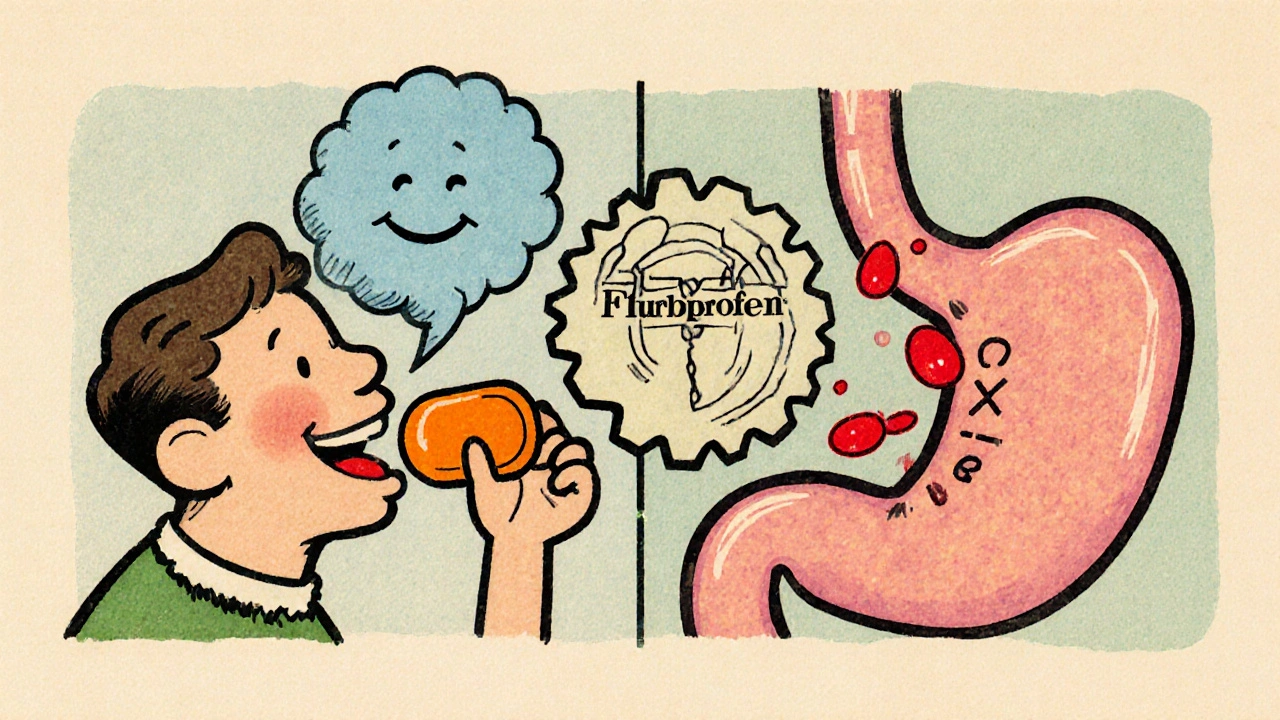
Flurbiprofen & Stomach Ulcers: Risks, Symptoms, and Safe Use
Learn how flurbiprofen can cause stomach ulcers, recognize warning signs, and use safe strategies to protect your gut while staying pain‑free.
When dealing with gastrointestinal bleeding, any loss of blood from the digestive tract, from the esophagus to the rectum. Also known as GI bleed, it can range from hidden occult loss to massive hemorrhage. A common source is peptic ulcer disease, a sore that forms in the stomach lining or duodenum and can erode nearby blood vessels. Another major driver is anticoagulant therapy, which thins the blood and makes even small injuries bleed more. These factors illustrate three semantic triples: gastrointestinal bleeding often results from peptic ulcer disease; anticoagulant therapy can increase the risk of gastrointestinal bleeding; managing gastrointestinal bleeding frequently requires endoscopic intervention. Understanding this web of causes helps you recognize warning signs early and seek help before the situation worsens.
Diagnosing a bleed starts with a careful history and physical exam, then moves to tools like endoscopy. Endoscopy lets doctors look inside the upper GI tract, pinpoint the bleeding spot, and often stop it with clips, cautery, or injection therapy. If the bleed originates lower in the colon, a colonoscopy may be needed. Blood tests reveal how much blood has been lost and whether the patient needs a transfusion. In severe cases, interventional radiology can block bleeding arteries when endoscopy fails. The treatment pathway reflects another set of triples: endoscopy enables direct visualization of gastrointestinal bleeding; endoscopic therapy can halt bleeding caused by peptic ulcer disease; blood transfusion supports patients with significant blood loss. Alongside procedural steps, doctors review medications—especially NSAIDs and anticoagulants—to adjust or pause them, reducing the chance of re‑bleeding.
Prevention focuses on the same risk factors that cause the bleed. If you take NSAIDs for chronic pain, consider using the lowest effective dose or switching to a safer alternative. For those on blood thinners, regular monitoring and dose adjustments can keep the balance between clot prevention and bleeding risk. Lifestyle tweaks—like limiting alcohol, quitting smoking, and eating a diet rich in fiber—support a healthy gut lining and lower ulcer formation. Recognizing the signs—black stools, vomiting blood, sudden weakness—means you can act fast. Below you’ll find a curated group of articles that dive deeper into each of these topics, from medication comparisons to practical tips for managing the aftermath of a bleed. Armed with this overview, you’re ready to explore the detailed resources that follow.
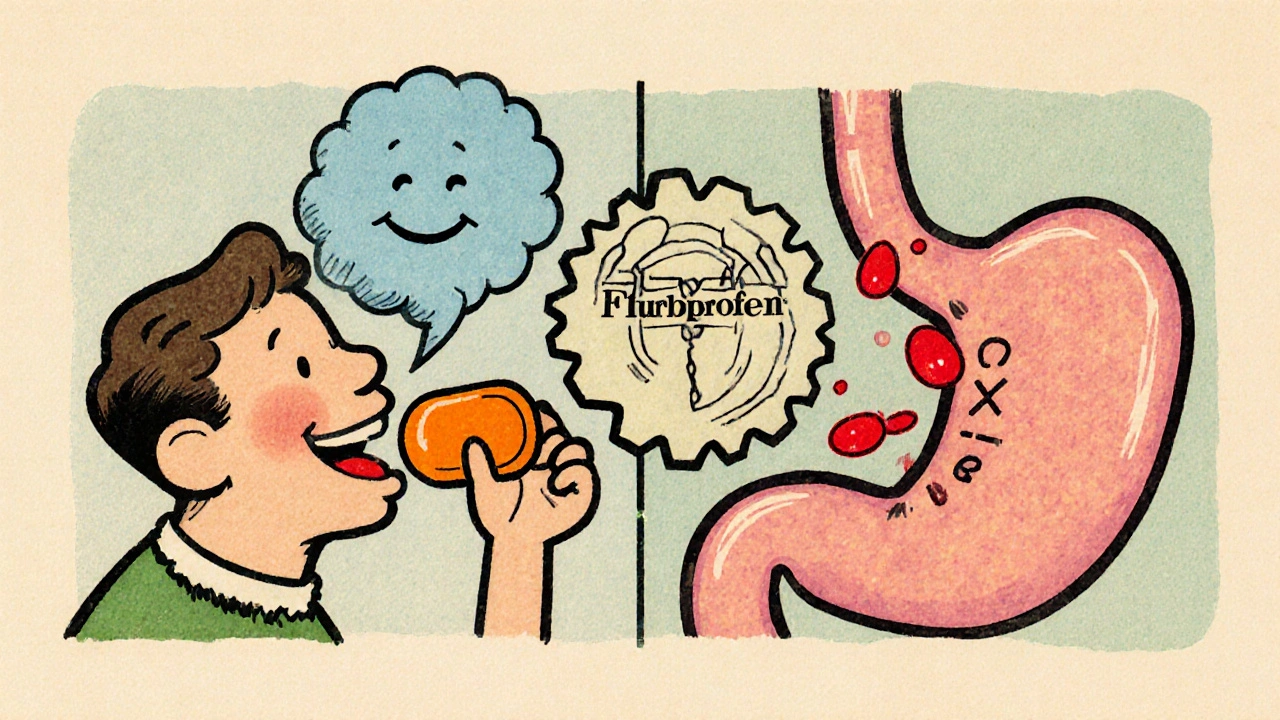
Learn how flurbiprofen can cause stomach ulcers, recognize warning signs, and use safe strategies to protect your gut while staying pain‑free.