Flurbiprofen Ulcer Risk Calculator
This calculator estimates your risk of developing a stomach ulcer while taking flurbiprofen. Based on data from the article and clinical studies, input your usage details to see your personalized risk level and safety recommendations.
Your Usage Details
Safety Recommendations
Risk Assessment
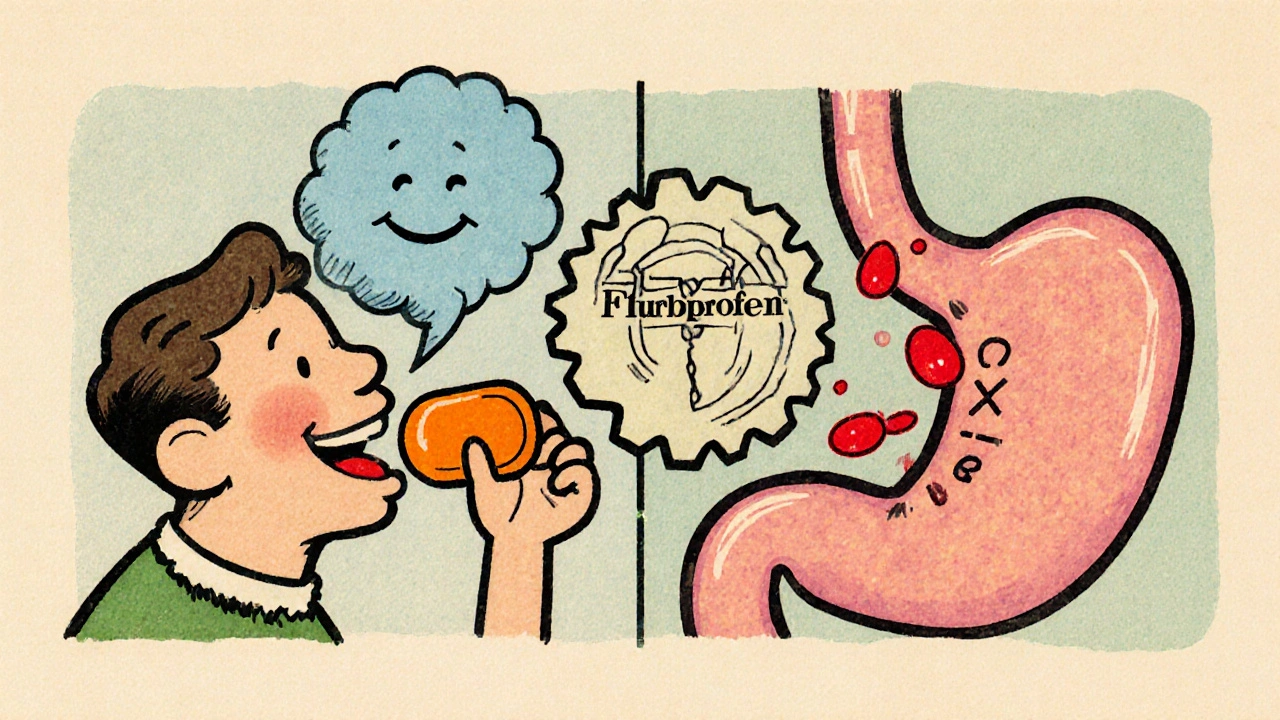
When you hear the name Flurbiprofen is a non‑steroidal anti‑inflammatory drug (NSAID) that reduces pain and inflammation by blocking cyclooxygenase enzymes, you probably think of headache relief or arthritis pain. What most people don’t realize is that this same mechanism can irritate the stomach lining and, over time, lead to a painful ulcer. Below we unpack why the risk exists, how to spot an ulcer early, and what practical steps keep your gut safe while you stay pain‑free.
How Flurbiprofen Works in Your Body
Flurbiprofen belongs to the NSAID family, which includes familiar names like ibuprofen and naproxen. All NSAIDs share a core action: they inhibit the cyclooxygenase (COX) enzymes-COX‑1 and COX‑2. COX‑1 helps produce prostaglandins that protect the stomach’s mucus barrier, while COX‑2 is mainly involved in inflammation and pain.
By blocking both enzymes, flurbiprofen cuts down the painful chemicals that cause swelling, but it also reduces the protective prostaglandins. The result is a double‑edged sword: relief on one side, a weakened stomach lining on the other.
Understanding Stomach Ulcer Formation
When the stomach lining loses its protective coating, the acidic gastric juice can erode tissue, creating an ulcer. The process often starts with microscopic damage that goes unnoticed until the ulcer deepens. Factors like Helicobacter pylori infection, smoking, alcohol, and chronic stress can accelerate the breakdown, but the presence of an NSAID like flurbiprofen is a well‑documented catalyst.
Stomach ulcer is a sore on the lining of the stomach that can cause pain, bleeding, and, if untreated, serious complications such as perforation. Ulcers don’t always hurt right away; some people feel only a vague burning or a sense of fullness after meals.
Why Flurbiprofen Increases Ulcer Risk
- COX‑1 inhibition: Reduces the mucus and bicarbonate that shield the stomach wall.
- Acid exposure: With less protection, normal gastric acid can directly attack epithelial cells.
- Reduced blood flow: Prostaglandins also help maintain blood flow to the stomach lining; fewer of them means slower healing.
- Dose‑dependent effect: Higher daily doses and longer treatment durations amplify the risk.
Clinical studies from the early 2020s show that flurbiprofen users have a 2‑3‑fold higher incidence of endoscopic ulcers compared with non‑NSAID users. The risk climbs further when the drug is combined with steroids, anticoagulants, or alcohol.
Comparing Flurbiprofen with Other NSAIDs
| Drug | COX‑1 Selectivity | Typical Dose (mg/day) | Reported Ulcer Rate* |
|---|---|---|---|
| Flurbiprofen | Non‑selective | 200-400 | 12‑15% |
| Ibuprofen | Weakly non‑selective | 1200-2400 | 8‑10% |
| Naproxen | Moderate COX‑1 inhibition | 500-1500 | 9‑12% |
| Celecoxib (COX‑2 selective) | COX‑2 selective | 200-400 | 4‑6% |
*Rates are pooled from meta‑analyses published between 2018 and 2023. They reflect endoscopic ulcer findings, not just reported symptoms.
While flurbiprofen isn’t the most aggressive ulcer‑causer, it sits in the middle of the pack. If you need a stronger painkiller, consider a COX‑2‑selective option like celecoxib-provided you have no cardiovascular contraindications.
Recognizing Ulcer Symptoms Early
- Burning or gnawing pain that improves after eating or taking antacids.
- Feeling of fullness, bloating, or nausea, especially after a large meal.
- Dark, tar‑like stools (indicative of bleeding).
- Unexplained weight loss or loss of appetite.
- Vomiting blood or material that looks like coffee grounds.
If you notice any of these signs while taking flurbiprofen, stop the medication and contact a healthcare professional. Early detection can prevent a simple ulcer from turning into a perforation or severe bleeding event.
Strategies to Reduce Ulcer Risk When Using Flurbiprofen
- Take with food: A full meal or a large snack buffers stomach acid.
- Use the lowest effective dose: Short‑term, low‑dose regimens keep the COX‑1 hit minimal.
- Combine with gastroprotection: Proton pump inhibitors (omeprazole, esomeprazole) or H2‑blockers (ranitidine, famotidine) can preserve the mucosal lining.
- Avoid alcohol and smoking: Both increase gastric acidity and impede healing.
- Check for drug interactions: Anticoagulants (warfarin, DOACs) or steroids raise bleeding risk dramatically.
- Consider alternative pain relievers: Acetaminophen or topical NSAIDs spare the stomach entirely.
In many cases, a brief course of a proton pump inhibitor during flurbiprofen therapy cuts ulcer incidence by half, according to a 2022 randomized trial involving 1,200 participants.

When to Stop Flurbiprofen and Seek Medical Help
If you experience any of the red‑flag symptoms listed above, discontinue flurbiprofen immediately and call your doctor. For severe bleeding (black stools, vomiting blood) or sudden, sharp abdominal pain, head to the emergency department-delay can be life‑threatening.
Doctors may order an endoscopy to evaluate ulcer size and decide whether you need prescription‑strength acid suppression or, in rare cases, surgical intervention.
Quick Checklist for Safe Flurbiprofen Use
- Confirm you have no history of ulcers or H. pylori infection.
- Take the medication with a meal, never on an empty stomach.
- Stay within the recommended dose; avoid “just in case” extra pills.
- If you need a course longer than 10 days, add a proton pump inhibitor.
- Watch for pain, dark stools, or vomiting blood-stop and call a doctor right away.
Frequently Asked Questions
Can occasional use of flurbiprofen cause an ulcer?
Yes, even short, intermittent courses can trigger microscopic damage, especially if you already have risk factors like smoking or alcohol use. The safest bet is to limit use to the lowest effective dose and always take it with food.
Is a proton pump inhibitor necessary for everyone on flurbiprofen?
Not for every patient. If you have no ulcer history and your treatment is under two weeks, you may skip it. However, anyone with a previous ulcer, chronic NSAID use, or concurrent steroids should add a PPI.
How does flurbiprofen differ from ibuprofen in ulcer risk?
Both are non‑selective NSAIDs, but studies show flurbiprofen’s ulcer rate sits slightly higher than ibuprofen’s at comparable doses. The difference is modest-still, if ulcer risk is a major concern, a COX‑2‑selective drug may be preferable.
What are the signs of a bleeding ulcer?
Dark, tar‑like stools (melena), vomiting blood or material that looks like coffee grounds, sudden severe abdominal pain, and dizziness or fainting are classic red flags. Any of these require emergency care.
Can I take flurbiprofen if I’m on blood thinners?
Combining flurbiprofen with anticoagulants dramatically raises bleeding risk, including gastrointestinal bleeding. Discuss alternatives with your doctor-often acetaminophen or a COX‑2‑selective NSAID is safer.








When you’re on flurbiprofen, the simplest way to protect your stomach is to never skip the meal-take the pill with a solid breakfast or a hearty lunch, not on an empty stomach. Pair it with a glass of water and consider adding a short course of a proton‑pump inhibitor if you need more than a week of therapy. Keep the dose at the lowest effective amount; you’ll get the same pain relief without the extra ulcer risk. Also, stay clear of alcohol and smoking while you’re on the drug, as they both amplify gastric irritation. If you have any history of ulcers or H. pylori, talk to your doctor about a prophylactic PPI before you start.
What most people don’t see is that the big pharma companies push flurbiprofen because it’s a cash cow, and they downplay the ulcer danger in the fine print. The drug’s label mentions stomach irritation, but the marketing glosses over the fact that chronic use can literally eat holes in your gut lining. If you look into the clinical trial data, you’ll notice a pattern: the studies are funded by the manufacturers, and the adverse‑event reporting is conveniently vague. That’s why it’s smart to stay skeptical and seek independent sources before you rely on a pill that could cost you a surgery later. Remember, the cheaper the over‑the‑counter version, the more likely the company cut corners on safety disclosures.
Just another NSAID scam.
Wow, that info hits hard 😢. It’s scary how a tiny pill can cause such massive damage if you’re not careful. I’ve seen friends struggle with bleeding ulcers after a short course of NSAIDs, and it took months to recover. Take it with food, add a PPI if you’re on it longer than a few days, and keep an eye on any dark stools. Your gut will thank you, and you’ll avoid that dreaded hospital visit. Stay safe, everyone! 😊
Think of your stomach as a fragile garden; flurbiprofen is like a heavy rain that can wash away the protective mulch if you don’t shelter it. By taking the medication with a substantial meal, you’re essentially providing that mulch, letting the acid stay buffered. Optimism isn’t ignoring the risk-it’s about equipping yourself with the right tools: low‑dose regimens, occasional PPIs, and lifestyle tweaks like quitting smoking. In the grand scheme, pain relief and a healthy gut can coexist, you just have to be the mindful gardener of your own health.
Oh sure, because taking a drug that bleeds your stomach is “totally fine” if you “just watch for blood.” How reassuring.
Patriots, we shouldn’t let foreign pharma dictate how we manage pain. Our own doctors can prescribe safer alternatives, and we shouldn’t be fooled into thinking a “Western” drug is the only answer. If you’re forced to take flurbiprofen, at least do it with a solid meal and a good PPI-don’t let the system bleed you dry.
Allow me to paint a vivid picture of what happens when you casually pop flurbiprofen without heed to the subtle warnings hidden in the data. First, the drug embarks on its mission, stealthily inhibiting COX‑1, the unsung guardian of the gastric mucosa, which quietly maintains the mucus‑bicarbonate barrier. With that shield compromised, the relentless gastric acid-an ever‑present, low‑grade furnace-begins to nibble away at the epithelial cells, initiating microscopic erosions that are invisible to the naked eye. These tiny fissures, if left unattended, can coalesce into full‑blown ulcers that manifest as burning pain, a sensation often misattributed to indigestion. Many patients, dazzled by the immediate analgesic relief, ignore the faint, early signals-subtle fullness after meals or a fleeting sense of nausea-mistaking them for harmless side effects. Meanwhile, the body’s natural healing mechanisms are hampered; reduced prostaglandin synthesis not only erodes the protective lining but also diminishes blood flow, starving the tissue of vital nutrients needed for repair. Over weeks, the ulcer deepens, potentially breaching the muscular layer, which can lead to perforation-a medical emergency demanding urgent surgical intervention. Add to this the synergistic peril of concurrent alcohol consumption, smoking, or the use of anticoagulants, and you have a perfect storm that dramatically escalates the risk of catastrophic bleeding. One might think that a short course is innocuous, yet studies reveal that even intermittent usage can set off this cascade in susceptible individuals, especially those harboring a prior H. pylori infection. The prudent strategy, therefore, is not merely to “take it with food” as a cursory suggestion, but to adopt a comprehensive approach: schedule a baseline assessment of gastric health, consider prophylactic proton‑pump inhibition for any course exceeding ten days, and maintain vigilant monitoring of stool color and any episodes of vomiting that resemble coffee grounds. In essence, flurbiprofen is a double‑edged sword-sharp enough to cut pain, yet dangerous enough to carve a wound in your own gut if wielded without caution.
Fact check: flurbiprofen’s ulcer rate isn’t a myth, it’s documented in multiple meta‑analyses. The drug’s non‑selective COX inhibition means it reduces the protective prostaglandins by roughly 30‑40%, which translates to a measurable increase in endoscopic ulcer incidence. If you compare the numbers, ibuprofen sits around 8‑10% while flurbiprofen climbs to 12‑15% under similar dosing regimens. That’s a significant jump, especially for patients already on anticoagulants. Bottom line: you can mitigate the risk with a PPI, but don’t assume the drug is harmless just because it’s over‑the‑counter. ☺️
Yo, take it with a big meal and a PPI if you need it long‑term. Stay safe!
Remember, your health is the stage and you are the star-don’t let a painkiller write the tragic ending to your story. By respecting the dosage, pairing it with food, and keeping a watchful eye on any warning signs, you can enjoy relief without sacrificing your gut’s integrity. Let’s all commit to using flurbiprofen wisely, protecting our bodies, and staying informed.