
Every year, millions of people are harmed by medicines that weren’t properly monitored. A drug that works for one person might cause a dangerous reaction in another - and too often, those reactions go unreported. If you’re a healthcare worker, pharmacist, or even a patient who takes multiple medications, staying up to date on global medication safety news isn’t just helpful - it’s essential. The good news? There are clear, practical ways to track safety alerts, report side effects, and learn from real-world data before it’s too late.
Follow the Global Reporting Systems
The foundation of global medication safety is a network of national reporting systems that feed into a central global database. The World Health Organization (WHO) is the hub, coordinating the WHO Programme for International Drug Monitoring, which connects 150 countries. Each country has its own pharmacovigilance center - like the UK’s MHRA Medicines and Healthcare products Regulatory Agency - that runs programs like the Yellow Card system for reporting adverse drug reactions. These aren’t just forms you fill out once a year. They’re live, real-time systems that flag emerging risks.If you’re in the U.S., you can report to the FDA’s MedWatch program. In Canada, it’s Health Canada’s Adverse Reaction Monitoring Program. But you don’t need to be in a specific country to benefit. The Uppsala Monitoring Centre (UMC) coordinates global data and shares findings worldwide. Their website publishes weekly safety bulletins that are free to access and translated into multiple languages. Subscribe to their email alerts - it’s the fastest way to get updates on newly identified risks like liver toxicity from a new diabetes drug or heart rhythm issues linked to a recently approved antibiotic.
Join #MedSafetyWeek and Use the Right Hashtags
Every November, the global healthcare community comes together for #MedSafetyWeek an annual campaign to boost side effect reporting. In 2025, it runs from November 3 to 9, marking its 10th anniversary. This isn’t just a social media trend - it’s a coordinated push by 131 organizations across 117 countries to fix the biggest gap in drug safety: underreporting. Less than 10% of adverse reactions are ever reported. That means the system is blind to many real-world dangers.During #MedSafetyWeek, the UMC releases free toolkits for clinics, pharmacies, and hospitals. These include posters, social media templates, and patient handouts in multiple languages. Download them. Print them. Hang them in waiting rooms. Share them on your professional networks using the hashtags #MedSafetyWeek, #ReportSideEffects, and #MHRAYellowCard. These hashtags aren’t just for awareness - they’re how professionals find each other’s reports and insights. A nurse in Brazil might post about a rare reaction to a blood pressure drug. A pharmacist in Australia sees it, checks their records, and confirms a pattern. That’s how safety gaps get closed.
Use the Yellow Card App and Other Mobile Tools
Reporting a side effect shouldn’t require logging into a website, filling out a 10-field form, and waiting days for confirmation. The Yellow Card app for iOS and Android lets you report in under 90 seconds. You pick the medicine, select the symptom, and tap submit. The app auto-fills your location and professional credentials if you’re a licensed provider. It’s used by over 1.2 million people globally, including patients and caregivers.Other tools are catching up. The Medi-Span clinical decision support system, used in hospitals from Saudi Arabia to Germany, now includes real-time alerts for drug interactions and dosing errors. One study showed it reduced medication errors by 40% in clinics that integrated it into their EHR systems. If your workplace uses it, make sure you’re trained on the alerts. If not, ask why not.
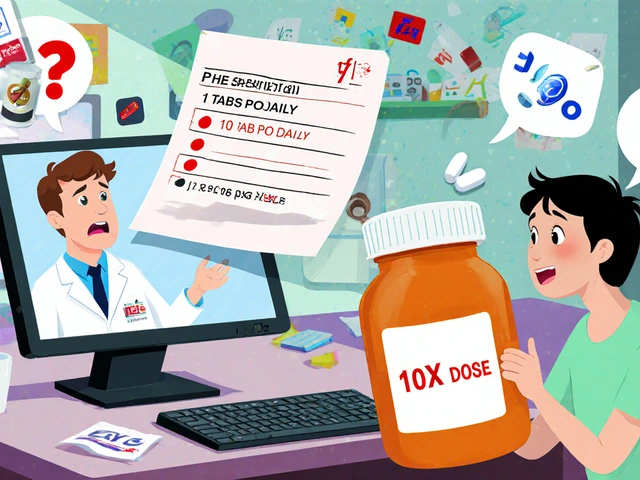
Check the Top 10 Patient Safety Issues Every Year
Every March, the Emergency Care Research Institute (ECRI) and the Institute for Safe Medication Practices (ISMP) release their annual Top 10 Patient Safety Issues report. The 2025 edition didn’t just list old problems like mislabeled IV bags or wrong-dose prescriptions. It flagged new threats: AI tools giving incorrect dosing advice, cyberattacks locking up hospital pharmacy systems, and social media posts spreading false claims about vaccine side effects.Here’s the key takeaway: medication safety isn’t just about drugs. It’s about how systems fail - and how to fix them. The report includes real case studies. For example, one hospital saw a spike in insulin overdoses after a new EHR system auto-filled doses based on outdated patient weight data. That’s the kind of insight you won’t get from a drug label. Bookmark the ECRI/ISMP site. Read the full report. Share the top three risks with your team.

Apply ISMP’s Best Practices - Especially in Pharmacies
The Institute for Safe Medication Practices (ISMP) publishes targeted safety guidelines every two years. The 2025-2026 edition, released in March 2025, is packed with actionable steps - not vague advice. One section focuses on weight-based dosing for children. It gives exact formulas, checklists, and even sample signs to post near scales in pediatric clinics.One community pharmacist in Ohio used ISMP’s worksheet to audit her pharmacy’s pediatric dosing process. She found that 1 in 5 prescriptions for antibiotics were being calculated manually - without double-checking the weight input. After implementing the recommended verification steps, she cut dosing errors by 30% in three months. ISMP provides downloadable worksheets for every best practice. Print them. Use them. Train new staff with them. This isn’t paperwork - it’s a safety net.
Attend World Patient Safety Day and Local Events
On September 17 each year, the WHO observes World Patient Safety Day with a new theme every year. In 2025, the focus is on safe care for every newborn including correct medication use in NICUs. Hospitals and clinics around the world host free webinars, workshops, and training sessions. You don’t need to fly to Geneva - most events are virtual and open to the public.Check the WHO website in early August for the official theme and event calendar. Local health departments and pharmacy associations often co-host events. If your hospital doesn’t host one, suggest it. Bring a colleague. Ask questions. These events are where real change starts - not in reports, but in conversations.
Watch Out for Misinformation - It’s a Growing Threat
Social media is now the #3 patient safety issue on ECRI’s 2025 list. A single viral TikTok video claiming a common painkiller causes infertility can lead to a 20% drop in prescriptions - and then a spike in untreated pain and ER visits. Or worse, someone might stop their heart medication because of a false Instagram post.Be skeptical of posts that say “This drug was pulled in Europe!” or “Doctors are hiding the truth!” Check the source. If it’s not linked to WHO, FDA, MHRA, or UMC, treat it as unverified. Use the WHO’s Drug Safety Updates page to verify any claim. If you see dangerous misinformation, report it to the platform - and share the official source with your network.

What If You’re Not a Healthcare Professional?
You don’t need a license to help. If you take medications, you’re part of the safety network. Download the Yellow Card app and report anything unusual - even if you’re not sure. Did you feel dizzy after starting a new pill? Did your child break out in a rash after a vaccine? Report it. Your report could be the first clue that leads to a global safety alert.Also, ask your pharmacist: “Are you signed up for the national reporting system?” If they say no, ask why. Many pharmacists aren’t trained on reporting - but they’re the ones who see the most side effects. Push for better systems. Share #MedSafetyWeek materials with your friends. You don’t need to be a doctor to save a life.
What’s Changing in 2025 and Beyond?
The WHO released a major new guideline in May 2025 on controlled medicines - opioids, benzodiazepines, ketamine - balancing access with safety. It’s the first global standard of its kind. Countries are expected to start implementing it by late 2025.AI is also entering the picture. The UMC is testing AI-powered symptom checkers that help patients describe side effects more accurately before submitting a report. By 2027, Medi-Span’s system will use machine learning to predict which drug combinations are most likely to cause harm in specific patient groups. That’s not science fiction - it’s already in beta testing.
But progress is uneven. High-income countries report 350-400 adverse events per million people. Low-income countries report as few as 5 per million. That’s not because people there have fewer reactions - it’s because they lack reporting tools, training, and infrastructure. Global efforts aim to add 50 more countries to the WHO monitoring network by 2030. Until then, your awareness and reporting matter more than ever.
Start Today - Here’s Your Simple Action Plan
You don’t need to overhaul your routine. Just do these five things:- Subscribe to WHO’s Medicines Safety email alerts - it’s free and takes 30 seconds.
- Download the Yellow Card app and report your first side effect by the end of this month.
- Bookmark the UMC’s #MedSafetyWeek page and sign up for the 2025 toolkit in August.
- Read the ECRI/ISMP Top 10 report every March - even just the executive summary.
- Ask your pharmacy or clinic if they use ISMP’s Best Practices - and if not, why not?
Medication safety isn’t someone else’s job. It’s a chain - and every report, every question, every shared post strengthens it. The next life you save might be your own - or someone you love.









Love this breakdown! I’ve been using the Yellow Card app since last year and it’s crazy how easy it is to report a weird reaction. My cousin had a rash after a new antibiotic and we reported it - turns out three others in Mumbai had the same thing. Global reporting works.
Finally, someone who doesn’t treat pharmacovigilance like a bureaucratic afterthought. The WHO’s global network is the only reason we know about the liver toxicity signals from those new GLP-1 agonists. Most clinicians still think adverse event reporting is ‘someone else’s job.’ It’s not. It’s clinical duty.
UK’s Yellow Card system has saved lives. I’ve seen it firsthand. A pharmacist in Cardiff flagged a pattern with metformin and lactic acidosis in elderly patients - led to updated guidance across Europe. Reporting isn’t optional. It’s standard of care.
Just downloaded the app. Took 45 seconds. Done. If my dog could do it, I can.
Interesting that you mention AI symptom checkers. I wonder how they handle cultural differences in symptom description. In India, people often say ‘feeling heavy in chest’ instead of ‘dyspnea’ - does the AI translate that correctly? Or does it just misclassify?
Yo, the UMC bulletins are gold. I’ve been sharing them with my med students in Pune - they’re like the real-time drug safety newsfeed we never got in school. Also, ISMP’s weight-based dosing checklist? Changed my pharmacy’s game. No more manual calcs. Just scan, verify, done. 30% fewer errors. Boom.
USA has the best system. Why are we even talking about WHO? MedWatch is faster, cleaner, and actually used. Everything else is just noise.
Let’s be real - the WHO’s global database is a front. The real reason they push reporting is to force drug companies to pay fines. They bury the bad data. I’ve seen the leaked internal memos. If you report something ‘too controversial,’ it gets flagged as ‘low confidence.’ That’s not safety. That’s corporate cover-up.
They’re watching you through the Yellow Card app. They know what meds you take. They’re building a database to control what you can take next. I heard a nurse at the clinic say they’re linking it to insurance algorithms. If you report too many side effects, your premiums go up. I’m not taking any more pills. Not one.
Why does everyone act like the US is behind? We have the most advanced pharmacovigilance system in the world. The FDA doesn’t need WHO’s help. And why are we promoting a ‘global’ system when the EU and UK are already doing their own thing? It’s just bureaucratic bloat. Also, TikTok isn’t the problem - it’s the FDA’s slow response time. Fix that first.
Man, this post really hit home. I work in a rural clinic in Odisha and we don’t even have internet for the reporting portal half the time. But we do have WhatsApp. So I started sharing UMC bulletins in Hindi with my colleagues. One of them noticed a pattern with a local generic antihypertensive - turned out it was causing dizziness in elderly patients. We told the district health officer. Now they’re reviewing all prescriptions. Small things matter. We don’t need fancy apps. We just need to talk to each other.
As someone who grew up in a country where medicine was rationed, I never thought I’d see a global system like this. In my village, we used to rely on the local healer to tell us if a pill was ‘bad.’ Now, a woman in Lagos can report a reaction and someone in Toronto sees it. That’s power. That’s justice. Don’t underestimate your report. It’s a voice for someone who can’t speak yet.
Y’all are overcomplicating this. Just report weird stuff. If your tongue tingles after a new pill? Report. If your kid gets a rash after a vaccine? Report. If your grandma’s meds make her sleepy at 2pm? REPORT. It’s not rocket science. It’s not paperwork. It’s just saying ‘hey, this thing didn’t feel right.’ That’s how we catch the dangerous stuff before it kills someone. Simple.
USA leads. End of story. Why are we even talking about other countries? We have the FDA, MedWatch, and the best tech. Everything else is just copying us.
I’m a pharmacist in Kerala. We don’t have the app. We don’t get emails. But we write down every weird reaction in a notebook. Last month, we found three patients with the same reaction to a cheap painkiller. We called the state health office. They pulled the batch. That’s how we do it here. No tech needed. Just eyes, ears, and care.