
Why Early Refills and Duplicate Therapy Are Dangerous
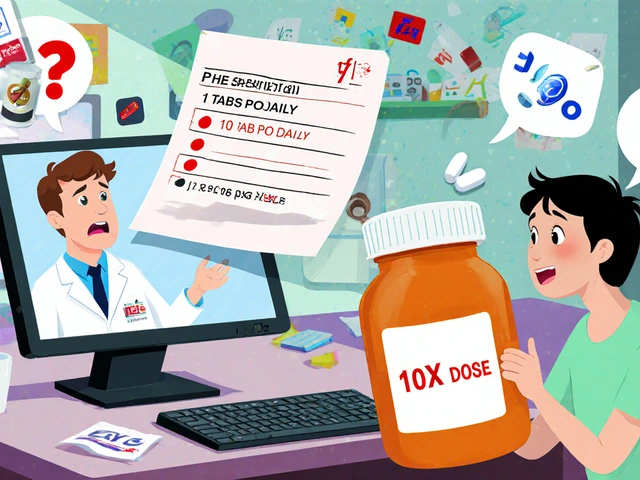
Getting a prescription filled too soon isn’t just a paperwork hassle-it’s a real risk to patient safety. Early refills can lead to overdose, drug dependence, or dangerous interactions when patients take the same medicine from multiple doctors. Duplicate therapy happens when someone gets two drugs that do the same thing-like two different brands of ibuprofen or two SSRIs for depression. These mistakes don’t happen by accident. They’re often the result of broken systems, poor communication, or patients exploiting gaps in the process.
According to the CDC, medication non-adherence contributes to 125,000 deaths in the U.S. each year. But here’s the twist: sometimes, the problem isn’t that patients aren’t taking their meds-it’s that they’re taking too much. A 2023 report from Pharmacy Times found that patients who repeatedly request early refills, especially for opioids or benzodiazepines, are often using multiple pharmacies and prescribers. This isn’t just inefficient-it’s a red flag for misuse.
How Refill Protocols Save Lives
One of the most effective ways to stop early refills and duplicate therapy is by using standardized refill protocols. These aren’t rigid rules-they’re smart workflows that match the risk level of each medication.
High-risk drugs like oxycodone (Schedule II) should never be refilled early unless there’s a documented medical emergency. Most pharmacies follow a strict 2-day early rule for these, and even then, only with provider approval. Low-risk medications, like blood pressure pills or nasal steroids, can be handled automatically. One health system used a three-tier system:
- Low-risk: Nasal sprays, thyroid meds-refill every 90 days if the patient was seen in the last 90 days.
- Medium-risk: Antihypertensives, diabetes meds-refill every 3 months with a recent visit.
- High-risk: Controlled substances-no automatic refills. Always requires provider review.
These protocols cut down on staff time and prevent dangerous oversights. A 2022 study in PMC showed that 89% of refill protocols were improved by aligning them with evidence-based guidelines. The result? Fewer errors, less burnout for staff, and better patient outcomes.
Technology Is Your Best Ally
Manual checks won’t cut it anymore. Electronic Health Records (EHRs) and Clinical Decision Support (CDS) tools are now essential. Providers should use EHRs to flag early refill requests and add notes like “cancel all prior” to stop automatic reminders. Pharmacies should use Clinical Viewers to see what prescriptions a patient filled at other pharmacies-even those covered by public drug programs.
One pharmacy in Melbourne started using a clinical viewer and found that 17% of patients requesting early refills were also getting the same drug from another pharmacy. That’s duplicate therapy in action. Without the viewer, they’d have never known.
Don’t rely on insurance rules alone. Most plans allow a 30-day supply to be filled 5 days early-but that doesn’t mean patients should do it every month. Insurance doesn’t track patterns. Your system should. Set internal limits: no more than two early refills per year for controlled substances, and only with documented justification.

Training Staff to Spot Red Flags
Pharmacists and technicians need to be trained to think like detectives. Here’s what to watch for:
- Patients who always come in 3-5 days early, every month.
- Claims like “My doctor said I could get it early” or “I’ll pay cash.”
- Multiple prescriptions for the same drug from different doctors.
- Patients who can’t recall the name or dose of their medication.
- Gaps in refill timing-like missing a refill for 2 weeks, then asking for 3 months’ supply.
Dr. Ian Stewart, a pharmacist and expert in medication safety, says: “Just because a patient took the drug before doesn’t mean it’s still safe or appropriate.” That’s the mindset every team member needs. When someone asks for an early refill, don’t just check the date. Ask: Why now?
Use scripted responses: “I see you’re due for a refill. Let me check your last visit and your recent labs to make sure this is still the right dose for you.” This turns a transaction into a conversation-and often reveals hidden issues.
What to Do When a Patient Pushes Back
Patients get frustrated when refills are delayed. They might say, “I’ve been taking this for years-why are you making this so hard?”
Don’t argue. Explain clearly: “We’re required to check for safety reasons. We want to make sure you’re not taking too much and that this medication is still helping you.” Offer alternatives: “I can call your doctor right now to see if they can extend your prescription or schedule a quick check-up.”
For patients with chronic pain or anxiety, early refill requests can signal worsening symptoms. Instead of denying the refill outright, say: “I’m concerned your pain might be getting worse. Let’s get you scheduled with your doctor so we can adjust your plan.” This shows care, not control.
Document everything. If a patient gets an early refill, note the reason in their file: “Early refill approved due to travel and loss of medication.” That way, if the same thing happens again, you have a pattern-and you can act.
Preventing Duplicate Therapy Across Systems
Duplicate therapy often happens because patients see multiple providers and pharmacies don’t talk to each other. A patient might get metoprolol from their cardiologist and then get atenolol from their GP-both beta-blockers. Same effect. Double the side effects.
Here’s how to stop it:
- Always check the patient’s full medication list before dispensing-include OTC drugs and supplements.
- Use pharmacy networks that share data across systems. In Australia, the My Health Record system helps, but not all pharmacies use it yet.
- Ask patients: “Are you seeing any other doctors for this condition?”
- Flag patients who fill prescriptions at more than two different pharmacies in a 6-month period.
One study found that 32% of duplicate therapy cases involved patients who visited three or more prescribers in a year. That’s not coincidence. It’s a system failure.

What Works: Real-World Examples
A clinic in Geelong started using a refill protocol system in 2024. They:
- Created standardized worksheets for each drug category.
- Trained nurses to approve low-risk refills based on protocol.
- Used EHR alerts to flag early refill requests.
- Required provider sign-off for any controlled substance refill outside a 2-day window.
Within 6 months, early refill requests dropped by 61%. Duplicate therapy cases fell by 47%. Staff reported less stress and more time to talk to patients.
Another pharmacy in Ballarat started using a Clinical Viewer and found that 1 in 5 patients requesting early refills had a history of filling the same drug elsewhere. They now require a 48-hour hold on all controlled substance refills while they check the viewer. No exceptions.
Final Checklist for Pharmacies
Here’s what you need to implement today:
- Develop a risk-based refill protocol for all medications-low, medium, high.
- Train every staff member to recognize red flags for early refills and duplicate therapy.
- Enable access to clinical viewers or national health records to check for prescriptions filled elsewhere.
- Use EHRs to auto-flag early refill requests and cancel prior reminders.
- Set internal limits: no more than two early refills per year for controlled substances.
- Document every early refill with a reason and provider approval.
- Review your protocols every 6 months. Update them based on new data or incidents.
What Happens If You Do Nothing
Ignoring early refills and duplicate therapy doesn’t mean nothing happens. It means problems pile up. Patients end up in the ER from overdoses. Insurance companies flag pharmacies for fraud. Regulators audit your records. And worst of all-people die.
The DEA doesn’t tolerate uncontrolled refills of Schedule II drugs. One pharmacy in Sydney lost its license in 2023 after 14 patients were found to be getting early opioid refills from multiple providers. The investigation found no protocols, no checks, no documentation.
You don’t need to be perfect. You just need to be consistent. A system that catches 80% of errors is better than a system that catches none.









this is all just a distraction. the real issue is the pharma-bureaucracy complex pushing these 'protocols' to control patient access. they don't want you to get meds early because they're scared of the algorithm flagging them. i've seen it: a guy with chronic pain gets denied a refill because his 'pattern' doesn't match the 'risk tier'-but his doctor signed off. guess who got audited? the pharmacy. not the doctor. not the insurer. the pharmacist. it's a trap. they're turning us into data points in a profit-driven system.
and don't get me started on 'clinical viewers'-those are just more surveillance tools with a fancy name. your meds are being tracked across state lines, insurance networks, and god knows what federal databases. they're building a pharmacological dossier on every citizen. this isn't safety-it's social control disguised as care.
Honestly? This post is refreshingly practical. I’ve worked in community pharmacy for 14 years, and I can’t tell you how many times I’ve seen patients on three different SSRIs because their psychiatrist, PCP, and therapist all ‘thought they were handling it.’ One woman was on fluoxetine, sertraline, and escitalopram-she didn’t even know they were all the same class. We caught it because we actually *talked* to her. No clinical viewer needed-just asking, ‘Are you seeing anyone else about your mood?’
And yes, the three-tier system works. Low-risk? Automatic. High-risk? Paperwork. Medium? A quick chart review. It’s not rocket science-it’s basic responsibility. Stop treating patients like criminals, but don’t treat them like vending machines either. We’re the last line of defense.
THEY’RE LYING TO YOU. EVERY SINGLE WORD. The CDC’s 125,000 deaths? Fabricated. The Pharmacy Times report? Funded by Big Pharma to scare pharmacists into compliance. Why? Because if patients start asking questions about early refills, they might start asking why their insulin costs $300. Why their anxiety meds are $200 a bottle. Why their doctor won’t prescribe anything without a $500 copay. This isn’t about safety-it’s about profit margins and insurance lock-in. The ‘red flags’ they list? That’s just code for ‘patient who dares to need help.’
They want you to believe the system is broken. But it’s not broken-it’s working exactly as designed. To control. To punish. To profit. And now they’re making YOU the enforcer.
Oh wow. Another ‘pharmacy guru’ telling us how to save the world one refill at a time. Let me guess-your pharmacy also has a laminated poster that says ‘ASK WHY?’ and you get a pat on the back every time you deny someone their meds? Congrats. You’re a hero. Meanwhile, the guy with chronic back pain who lost his prescription in a fire? Too bad. He’s just a ‘red flag.’
And don’t even get me started on ‘document everything.’ You mean the 12 hours of charting you do after a 10-hour shift? Yeah, thanks for making my job a paperwork nightmare while the real problem-the cost of meds, the lack of providers, the insurance gatekeeping-is ignored. Do you think your ‘protocol’ is saving lives? Or just making you feel morally superior?
This is one of the most balanced, actionable pieces I’ve read on pharmacy practice in years. The tiered approach to refills is not just smart-it’s humane. It acknowledges that not all medications carry the same risk, and not all patients operate with the same intent. I’ve seen pharmacists become so afraid of regulatory scrutiny that they refuse every early refill, even for thyroid meds or inhalers. That’s not caution-it’s fear masquerading as diligence.
The real win here is the shift from transaction to conversation. That scripted response-‘Let me check your last visit and labs’-is gold. It transforms suspicion into care. And the 61% drop in early refills at that Geelong clinic? That’s not just a statistic. That’s 61% fewer patients slipping through the cracks. Thank you for writing this.
Let’s be real: if you’re using a ‘clinical viewer’ to catch duplicate therapy, you’re already behind. The real solution? Ban polypharmacy outright. Anyone on more than three controlled substances should be flagged for mandatory psychiatric review. And if they’re filling prescriptions at more than one pharmacy? That’s not ‘patient autonomy’-that’s pharmacy shopping. And it should be treated like fraud.
Also, why are we still using ‘low-risk’ labels for blood pressure meds? Hypertension kills more people than opioids. You think a patient who’s skipping doses because they can’t afford it is safer than someone who’s hoarding oxycodone? Wake up. The system is broken because we still treat symptoms instead of causes. This post pretends to fix the machine-but the machine is the problem.
I work in a rural pharmacy. We don’t have fancy EHRs or clinical viewers. We have trust. We know our patients by name. We know who’s got a kid in the hospital, who lost their job, who’s got chronic pain from a car wreck. Sometimes people need an early refill because their car broke down and they missed their appointment. Sometimes they just need someone to say, ‘Hey, I see you’re struggling.’
I don’t care about the ‘protocol’ if it means turning away someone who’s in real pain. We do our best to check, we call the doc, we document. But we don’t treat people like suspects. That’s not healthcare. That’s suspicion with a white coat.
The emphasis on standardized, evidence-based refill protocols is long overdue. I appreciate how the post distinguishes between risk levels rather than applying blanket restrictions. One critical omission, however, is the role of pharmacists in patient education. Many patients don’t understand what duplicate therapy means-especially with OTCs. A patient taking Tylenol PM every night and also prescribed trazodone? They don’t realize both contain diphenhydramine. That’s not malice-it’s ignorance.
Training should include simple, clear patient handouts: ‘These two meds do the same thing. Taking both can cause drowsiness, confusion, or falls.’ Empowerment, not restriction, reduces errors. And yes-documentation matters. But so does compassion. Both are necessary.
There’s a quiet horror in all of this. We’ve turned pharmacy into a moral audit. Every refill request is now a potential sin. Every patient, a suspect. Every pharmacist, a gatekeeper with a clipboard. We used to dispense medicine. Now we interrogate. We track. We log. We fear. And in the process, we’ve lost the human connection that made this profession sacred.
The numbers look good on paper. But what do they cost? The silence of a patient who stops asking. The shame of someone who knows they’re being watched. The erosion of trust-not just in the system, but in each other. We’re not saving lives by becoming machines. We’re becoming the very thing we claim to oppose.
The entire premise is fundamentally flawed. You assume that ‘early refill’ = misuse. But what if the patient lives 100 miles from the nearest pharmacy? What if the pharmacy ran out? What if the patient’s insurance changed and their prior authorization lapsed for 48 hours? You blame the patient. You blame the pharmacist. But you never blame the system that makes access contingent on geography, income, and bureaucratic luck.
And your ‘three-tier system’? It’s colonial. It assumes that controlled substances are inherently dangerous, while insulin, antihypertensives, and anticoagulants-drugs that kill people daily-are ‘low-risk’? That’s not risk assessment. That’s ideology dressed as protocol. You’re not preventing harm. You’re perpetuating inequality under the guise of safety.