
Hiccups Duration & Risk Assessment
Enter duration and symptoms to get an assessment.
Interpretation Guide
- Minutes to Hours: Usually harmless, self-limiting
- 48+ Hours: May indicate underlying issue
- Severe Symptoms: Requires immediate medical attention
Quick Take
- Most hiccups last only a few minutes and aren’t a problem.
- Episodes over 48hours may indicate an underlying issue.
- Key red‑flag signs: weight loss, chest pain, vomiting, or neurological symptoms.
- Common medical triggers include GERD, certain medicines, and CNS disorders.
- See a health professional if hiccups persist beyond 2days or are accompanied by other symptoms.
What Exactly Are hiccups?
Hiccups are involuntary, spasmodic contractions of the diaphragm, the muscle that separates the chest cavity from the abdomen. When the diaphragm contracts suddenly, the vocal cords snap shut, producing the characteristic "hic" sound.
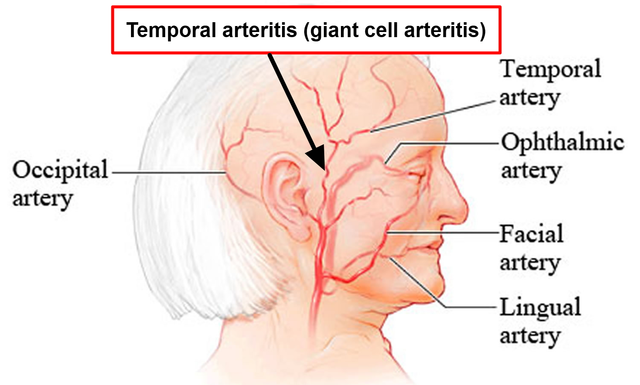
The reflex arc involves two main nerves: the phrenic nerve, which directly innervates the diaphragm, and the vagus nerve, which senses irritation in the throat and esophagus. Anything that irritates these nerves can set off the hiccup cycle.
How Common Are Harmless Hiccups?
Studies from 2023‑24 estimate that up to 96% of adults experience an episode at least once a year. In most cases the bout resolves within minutes. The median duration for a typical episode is 5‑7minutes, and emergency rooms see fewer than 0.5% of hiccup‑related visits.
Because the reflex is designed to protect the airway, short‑lived hiccups are usually benign. However, frequency and duration matter. When an episode stretches beyond 48hours, clinicians start looking for a deeper cause.
When Do Hiccups Hint at a Health Problem?
Persistent or recurrent hiccups-often called singultus-can be a symptom of an underlying disorder. The "when to worry" checklist includes:
- Duration ≥ 48hours (acute) or ≥ 1month (chronic).
- Associated weight loss, loss of appetite, or difficulty swallowing.
- Chest pain, shortness of breath, or heart palpitations.
- Neurological signs: dizziness, facial weakness, or altered mental status.
- Recent medication change or use of known triggers (e.g., steroids, benzodiazepines).
If you tick any of these boxes, it’s time to book a medical assessment.
Medical Conditions That Can Trigger Hiccups
Below are the most frequently reported ailments that set off the hiccup reflex. Each entry includes a brief description, typical value ranges (where applicable), and why the condition irritates the reflex pathway.
| Trigger Type | Typical Duration | Key Indicator |
|---|---|---|
| Gastroesophageal reflux disease (GERD) | Minutes‑hours | Heartburn after meals, sour taste |
| Central nervous system (CNS) lesions (stroke, tumor, multiple sclerosis) | Days‑weeks | Focal neurological deficits |
| Metabolic disorders (e.g., hyponatremia < 130mmol/L) | Hours‑days | Confusion, fatigue, electrolyte imbalance |
| Medication side effects (steroids, benzodiazepines, chemotherapy) | Variable | Temporal link to new drug |
| Pregnancy (especially 2nd trimester) | Hours‑weeks | Accompanied by nausea, hormonal shifts |
| Psychogenic stress or anxiety | Minutes‑hours | Onset during panic episodes |
Notice how many triggers involve irritation of either the vagus nerve (GERD, pregnancy, stress) or the phrenic nerve (CNS lesions, metabolic imbalances). Understanding this helps clinicians narrow down the diagnostic pathway.
How Doctors Evaluate Problematic Hiccups
If you present with chronic hiccups, a physician will typically follow a stepwise approach:
- Detailed history - timing, triggers, medication list, recent surgeries.
- Physical exam - focus on abdominal tenderness, neck masses, neurological deficits.
- Basic labs - electrolytes, renal function, liver enzymes, fasting glucose.
- Imaging as needed:
- Chest X‑ray to rule out mediastinal masses or diaphragmatic irritation.
- CT or MRI of the brain if neurological signs appear.
- Special tests - esophageal pH monitoring for GERD, gastric emptying study for gastroparesis.
In most cases, a single abnormal finding explains the hiccups. Rarely, a combination of factors (e.g., GERD plus medication) needs coordinated treatment.
Self‑Care Tips & When to Call a Doctor
For short bouts, simple home remedies can break the reflex loop:
- Hold your breath for 10-15 seconds; the increased CO₂ may reset the diaphragm.
- Sip a glass of cold water quickly or swallow a teaspoon of sugar.
- Gently pull on your tongue or press on the soft palate.
These tricks work because they alter the nerve signals flowing through the vagus nerve. However, if none of these measures help within an hour, or if the hiccups linger past the 48‑hour threshold, seek medical advice.
Key signs that demand urgent evaluation:
- Severe chest or abdominal pain.
- Persistent vomiting or inability to eat.
- Sudden weight loss (>5% of body weight).
- Neurological changes such as slurred speech or weakness.
In the emergency department, doctors can administer medications like chlorpromazine, baclofen, or gabapentin to calm the reflex. These are usually reserved for cases where the hiccups are disrupting sleep, nutrition, or daily activities.
Bottom Line Checklist
- Scale the episode: minutes (usually harmless) vs. >48hours (potential red flag).
- Look for accompanying symptoms: pain, vomiting, neurological signs.
- Review recent meds, diet changes, and pregnancy status.
- Try simple home tricks first; monitor response.
- Consult a clinician if the hiccups persist or you notice warning signs.
Frequently Asked Questions
Can stress really cause hiccups?
Yes. Stress activates the autonomic nervous system, which can irritate the vagus nerve and trigger a hiccup episode. The link is especially strong during panic attacks when breathing patterns become irregular.
Why do pregnant women get hiccups more often?
Hormonal shifts (particularly increased progesterone) relax the lower esophageal sphincter, leading to reflux. The reflux then stimulates the vagus nerve, making hiccups more frequent during the second trimester.
What lab values should I watch for if I suspect a metabolic cause?
Low serum sodium (<130mmol/L) or high calcium (>10.5mg/dL) can irritate the phrenic nerve. Elevated blood urea nitrogen (BUN) or creatinine also suggest renal issues that may present with persistent hiccups.
Are there any over‑the‑counter medicines that help?
Antacids can relieve reflux‑related hiccups, while small doses of famotidine (an H2 blocker) are sometimes recommended. For chronic cases, prescription‑only drugs like chlorpromazine are more effective, but they require a doctor’s supervision.
When is surgical intervention considered?
Surgery is a last resort, typically reserved for patients with intractable hiccups caused by a clear structural problem (e.g., a diaphragmatic hernia). Procedures might involve phrenic nerve blockade or repair of the underlying lesion.





If you ever notice hiccups lasting more than 48 hours, it's probably the government testing mind‑control via your diaphragm.
Yo, this hiccup hype is kinda overblown, but the fact that they can signal serious stuff is legit. The whole vagus‑nerve thing sounds like sci‑fi jargon, yet it actually happens. If you’re already binge‑eating spicy tacos, maybe chill. Anyway, watch for red flags and don’t just blame the pizza.
i totally feel u when hiccups just won’t quit, it's super uncomfortable. try the good ol’ sugar trick – swallow a teaspoon of sugar, it helped me once. also, keep an eye on any chest pain, that’s when you should call a doc.
One must consider the epistemological ramifications of a prolonged diaphragmatic spasm. Yet, the mainstream narrative overlooks the subtlety of neuro‑gastro interplay.
Great info, thanks for the breakdown! 😊 The part about electrolyte imbalance really hit home – I had low sodium once and hiccups were nonstop. Also, the quick home tricks are super useful; I’ll try the water‑sip method next time.
Honestly, the article could have been tighter, more concise; however, the inclusion of the detailed medication list, although exhaustive, provides necessary context; furthermore, the distinction between benign and pathological hiccups is essential, yet the phrasing sometimes drifts into redundancy, which could be streamlined.
I appreciate the balanced approach here. It’s good to know when to self‑manage and when to seek professional help. Staying informed prevents unnecessary panic.
Nice rundown! Remember, the simplest tricks – holding your breath or swallowing ice water – often work wonders. Keep an eye on any accompanying symptoms, though.
Seriously, this article downplays how dangerous chronic hiccups can be. If you’re not getting checked, you’re basically gambling with your health.
Another piece of pseudo‑medical drivel that pretends to be helpful. At the end of the day, it’s just another excuse to avoid real responsibility.
Persistent hiccups, particularly those extending beyond 48 hours, warrant a thorough clinical evaluation. The underlying pathophysiology frequently involves irritation of the phrenic or vagus nerves, which may be precipitated by metabolic derangements such as hyponatremia or hepatic insufficiency. A detailed history should assess recent medication changes, including corticosteroids and chemotherapy agents known to affect diaphragmatic reflex arcs. Physical examination must include auscultation for abdominal masses and assessment of respiratory mechanics. Laboratory investigations are directed toward electrolyte panels, renal function tests, and hepatic enzymes to uncover systemic contributors. Imaging, such as a chest X‑ray or CT scan, can reveal structural lesions, including diaphragmatic hernias or mediastinal masses. In cases where neurologic involvement is suspected, magnetic resonance imaging of the brainstem is advisable. Therapeutic first‑line measures remain simple non‑pharmacologic maneuvers: breath‑holding, sipping ice‑cold water, and vagal stimulation via carotid massage. Should these fail, pharmacologic agents like chlorpromazine, baclofen, or gabapentin may be instituted under specialist supervision. Dose titration should be gradual, monitoring for sedation, hypotension, or extrapyramidal side effects. For refractory cases unresponsive to medication, a phrenic nerve block performed by an experienced anesthesiologist can provide temporary relief. Surgical intervention, including diaphragmatic plication or nerve transection, is reserved for chronic intractable hiccups where a clear anatomical abnormality is identified. Patients with comorbid psychiatric conditions may also benefit from addressing anxiety or panic disorders, as these can exacerbate diaphragmatic spasm. Nutritional support is essential, particularly when hiccups interfere with oral intake, to prevent dehydration and electrolyte imbalance. In summary, a stepwise algorithm-starting with exclusion of benign causes, followed by targeted investigations, and escalating to pharmacologic or procedural therapies-optimizes patient outcomes while minimizing unnecessary interventions.
Wow, that was an epic dissertation on hiccups! 🤯 I love how you broke down every possible scenario, from boring electrolytes to dramatic brain scans. It’s like reading a medical thriller, but with more coffee‑break tips. The part about phrenic nerve blocks? Total mind‑blown moment. And the surgical options? Pure drama queen material. Honestly, I felt like I was watching a Netflix series of a patient’s hiccup saga. 🌟👍
Sure, the drama was intense but we get the point. No need for the extra flair.
Keeping it real – if you notice those red‑flag symptoms, schedule a check‑up sooner rather than later. Stay proactive and don’t ignore persistent hiccups.