
Metformin & Alcohol Risk Calculator
Personal Risk Assessment
This tool helps you understand your individual risk of lactic acidosis when combining metformin with alcohol. Based on your health factors and drinking habits, it provides a risk level recommendation.
Your Risk Assessment
Select your details above to see your personalized risk assessment.
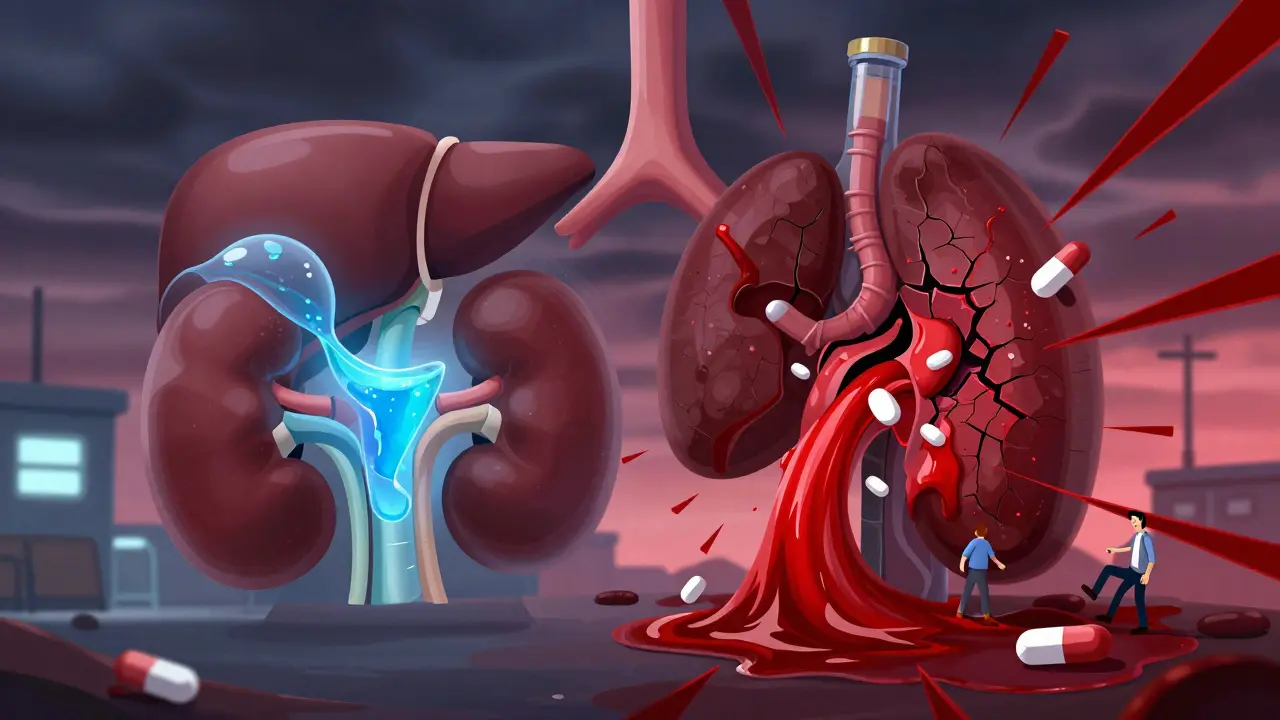
Combining metformin and alcohol might seem harmless-after all, many people with type 2 diabetes enjoy an occasional drink. But behind that glass of wine or beer is a rare, silent danger: lactic acidosis. It’s not common, but when it happens, it can be deadly. And the risk doesn’t just come from heavy drinking. Even moderate alcohol use can tip the balance in people taking metformin, especially if their kidneys aren’t working at full strength.
What is lactic acidosis, and why does it matter?
Lactic acidosis is when your blood becomes too acidic because too much lactic acid builds up. Normally, your body makes small amounts of lactic acid during exercise or when oxygen is low. Your liver and kidneys clear it out. But when that system gets overloaded, things go wrong fast.
Metformin slows down how your liver makes sugar-and in the process, it slightly increases lactic acid production. Alcohol does the opposite: it shuts down your liver’s ability to clear lactic acid. Put them together, and your body can’t keep up. Blood lactate levels climb past 5 mmol/L, pH drops, and your organs start struggling. This isn’t a slow decline-it can crash within hours.
Death rates for lactic acidosis linked to metformin (called MALA) range from 30% to 50%. That’s why the FDA put a black box warning on metformin labels-the strongest warning they give. It’s rare: about 0.03 cases per 1,000 people per year. But when it hits, it hits hard.
How alcohol makes metformin dangerous
Metformin doesn’t cause lactic acidosis on its own in healthy people. But alcohol changes the game. Here’s how:
- Alcohol uses up NAD+-a key molecule your liver needs to break down lactic acid. Without it, lactic acid piles up.
- Metformin reduces liver glucose production, which indirectly pushes your body to rely more on anaerobic metabolism-another source of lactic acid.
- Both hit the kidneys. Metformin is cleared mostly through the kidneys. Alcohol dehydrates you and can reduce kidney function temporarily, making it harder for your body to flush out metformin.
It’s not just about how much you drink-it’s about how your body handles it. A 65-year-old man with normal kidney function died from lactic acidosis after binge drinking 10 shots of vodka while on metformin. He didn’t have diabetes complications. He didn’t have kidney disease. Just alcohol + metformin.
Who’s most at risk?
You don’t need to be a heavy drinker to be in danger. But certain factors make lactic acidosis more likely:
- Chronic or binge drinking-4+ drinks in 2 hours for women, 5+ for men. This is the biggest red flag.
- Impaired kidney function-even mild decline raises risk. Your eGFR should be checked regularly if you’re on metformin.
- Older age-kidney function drops naturally after 60.
- Heart failure or liver disease-both reduce your body’s ability to manage acid levels.
- Dehydration-from alcohol, illness, or not drinking enough water.
Even people with no known risk factors have developed MALA after a single night of heavy drinking. That’s why doctors don’t give a “safe” number of drinks. The warning says “avoid excessive alcohol”-but no one defines what that means in exact terms.
What do experts really say?
The American Diabetes Association says to avoid “excessive alcohol” while on metformin. But they don’t say how much is too much. The European Medicines Agency is clearer: acute alcohol intoxication is a known trigger.
Dr. Robert A. Rizza from Mayo Clinic says moderate drinking-1 drink a day for women, 2 for men-might be okay for some people with normal kidneys. But he adds: “Any binge drinking or chronic heavy use? That’s a dangerous mix.”
Dr. John B. Buse, former ADA president, puts it bluntly: “The symptoms are vague-nausea, muscle pain, fatigue. Patients think it’s a hangover. By the time they get to the ER, it’s often too late.”
And here’s the scary part: 68% of patients who ended up in the hospital with MALA didn’t realize their symptoms were serious. They thought, “I just drank too much.”
Real stories from real people
On Healthline’s diabetes forum, a user named DiabetesWarrior42 wrote: “I had six beers with dinner. Two hours later, I couldn’t stand up. My legs were cramping. My heart was racing. They found my lactate at 6.2 mmol/L. I spent three days in ICU.”
Another Reddit user, SugarFreeLife, shared: “My doctor said two glasses of wine is fine. Then I had 10 shots at a bachelor party. I couldn’t breathe. My muscles locked up. I thought I was having a panic attack. Turns out, I was dying.”
GoodRx surveyed metformin users. 78% cut back on alcohol because they were scared of lactic acidosis. 42% said that’s their #1 concern-more than weight gain or stomach upset.
What should you do?
There’s no official safe limit. But here’s what works in real life:
- Avoid alcohol entirely during the first 4-8 weeks after starting metformin. Your body is adjusting. Don’t add stress.
- Never drink on an empty stomach. Alcohol + metformin can also cause low blood sugar. Eat before you drink.
- Avoid binge drinking at all costs. That’s the fastest path to trouble.
- Know the warning signs: unusual muscle pain, trouble breathing, dizziness, nausea, vomiting, stomach pain, feeling cold, or rapid heartbeat. If you feel this way after drinking, go to the ER-don’t wait.
- Get your kidney function checked yearly. If your eGFR drops below 45, talk to your doctor about alternatives.
And here’s something most people don’t know: both metformin and alcohol can cause vitamin B12 deficiency. Long-term users lose 7-10% of their B12 levels every year. Alcohol makes it worse. Low B12 can lead to nerve damage, memory problems, and fatigue-symptoms that look like diabetes complications. Get tested if you’ve been on metformin for more than 3 years.

Are there safer diabetes drugs?
Yes. Newer drugs like GLP-1 agonists (semaglutide, liraglutide) and SGLT2 inhibitors (empagliflozin, dapagliflozin) don’t carry lactic acidosis risk. They’re often used when metformin isn’t suitable. But they’re more expensive, and metformin still works better for most people.
Metformin is the most prescribed diabetes drug in the world-over 150 million prescriptions in the U.S. alone each year. It’s cheap, effective, and reduces heart disease risk. The lactic acidosis risk is tiny compared to its benefits. But that doesn’t mean you can ignore it.
Phenformin, metformin’s predecessor, was pulled off the market in 1978 because 40-64 people per 100,000 got lactic acidosis. Metformin’s rate? About 0.03 per 1,000. That’s 100 times safer. But safety doesn’t mean zero risk. It means you have to be smart.
What’s changing in 2025?
The FDA approved new extended-release metformin formulations in 2023 that cause less stomach upset-but the lactic acidosis warning is unchanged. The same risk applies.
A major study called the MALA-Prevention Study started in January 2024. It’s tracking 5,000 metformin users to finally answer: What level of alcohol consumption is actually dangerous? Results won’t be out until late 2025. Until then, the advice remains: when in doubt, skip it.
Experts like Dr. Silvio Inzucchi from Yale say we need better guidelines. Right now, doctors guess. Patients guess. That’s not good enough.
Bottom line
You don’t have to quit alcohol forever. But if you’re on metformin, you need to treat alcohol like a controlled substance-not a casual habit. One drink? Maybe okay. Two drinks in a row? Risky. A whole night of drinking? Dangerous. Your liver and kidneys are already working hard to keep your blood sugar stable. Don’t ask them to handle more.
Know your body. Know the signs. Talk to your doctor. And if you ever feel like you’re slipping into something worse than a hangover-get help immediately. Lactic acidosis doesn’t wait.






I’ve been on metformin for 7 years and only had one glass of wine with dinner-never binged, never skipped meals. My kidneys are fine, my A1C is 5.8. But I still check the labels now. It’s not about fear-it’s about respect for what your body’s doing. If you’re gonna drink, be mindful. Not because the system’s out to get you, but because your liver’s already working overtime.
Lactic acidosis? More like a pharmacokinetic nightmare. Metformin inhibits hepatic gluconeogenesis via AMPK activation and mitochondrial complex I suppression, which elevates NADH/NAD+ ratio → shifts pyruvate → lactate. Alcohol? It’s a competitive inhibitor of alcohol dehydrogenase, depletes NAD+, and suppresses hepatic gluconeogenesis via glucagon suppression. The synergy isn’t just additive-it’s multiplicative. You’re essentially creating a metabolic trap. Anyone who thinks ‘one drink’ is safe hasn’t read the 2021 JAMA Internal Medicine meta-analysis on lactate kinetics in T2DM patients under ethanol load.
Alcohol is sin. Metformin is medicine. Mixing sin with medicine is asking God for punishment. People in America think everything is okay if it feels good. But body is temple. Drink less. Think more. God sees everything.
While I appreciate the general tone of this post, I must emphasize that the FDA's black box warning is not merely a precaution-it is a clinical imperative grounded in pharmacovigilance data from the 1990s to present. Furthermore, the concomitant use of metformin and ethanol induces a state of type B lactic acidosis, which is distinct from type A (hypoxic) in etiology but identical in pathophysiological outcome. The absence of a quantified "safe" threshold is not an oversight-it is a deliberate regulatory stance reflecting the non-linear dose-response curve of ethanol-induced metabolic decompensation in susceptible populations. Also: 🧠💡
My dad was on metformin and had a glass of wine every night. He never knew the risk. He passed away from something that looked like a stroke but was actually MALA. No one told him. No one warned him. I’m so glad this post exists. If you’re reading this and you’re on metformin-ask your doctor. Not just once. Ask again next year. And if you’re a doctor? Don’t assume they know. Say it plainly. "Don’t binge. Don’t drink on empty. And if you feel weird after a drink-go to the ER. Don’t wait."
As someone who’s lived in both India and the U.S., I’ve seen how cultural attitudes toward alcohol and medication differ wildly. In India, people often see metformin as a "weight-loss pill" and drink casually, thinking "it’s just sugar control." In the U.S., people overthink it and avoid all alcohol-even a single glass with dinner-out of fear. The truth? It’s not black and white. A healthy 40-year-old with eGFR >60 and no liver issues? One drink, with food, once a week? Probably fine. But if you’re 70, dehydrated, and binge-drinking on weekends? You’re playing Russian roulette with your kidneys and liver. The real issue isn’t the drug or the drink-it’s the lack of clear, culturally sensitive education. We need more doctors who speak plain language, not just jargon.
EVERYTHING IS A LIE. The FDA? Controlled by Big Pharma. The ADA? Paid off. Metformin was NEVER meant to be a long-term solution-it was a stopgap. And now they’re using it to keep people dependent while hiding the REAL cause of diabetes: sugar, processed food, and corporate greed. And alcohol? They’re using it as a scapegoat so you don’t ask why your insulin is failing. They don’t want you to know that metformin was originally derived from French lilac-a plant that lowers blood sugar NATURALLY. But you can’t patent a plant. So they made a synthetic version, slapped a black box on it, and now you’re terrified of wine. Wake up. The real danger isn’t alcohol-it’s the system that profits from your fear.
In India, we have a tradition of Ayurveda and natural remedies. Metformin is a Western chemical. Alcohol is a Western vice. To mix them is to disrespect both our ancestral wisdom and modern science. Our elders would never consume such combinations. Why do we, the younger generation, think we know better? We must return to balance-diet, yoga, and discipline. Not pills and cocktails.
i’ve been on metformin for 5 years and i only drink on weekends, like 1 glass of wine. i eat first, i drink slow, and i check my sugar. no issues. but i do feel weird sometimes after and i just think "oh, maybe i drank too much"-now i know it might’ve been something else. thanks for this, really helpful. also, my doctor never mentioned the b12 thing. gonna get tested next week.
Oh wow, so now I’m supposed to feel guilty for having a margarita on Friday? Cool. I’ll just sip it slowly while staring at my kidneys like they’re about to betray me. 🥴💀 Meanwhile, my doctor says "moderate" and I say "I’m not a lab rat." But hey, thanks for the B12 tip-that’s actually useful. I’ve been tired as hell for a year. Maybe it’s not my ADHD meds after all.
Okay, real talk: I used to think "one drink" was fine. Then I got sick after a birthday party-cold sweats, chest tightness, couldn’t breathe. Thought I was having a panic attack. Turned out my lactate was 5.8. ICU. Three days. Now I don’t drink at all. But I also started walking 10k steps a day, eating more veggies, and taking B12 supplements. I feel better than I have in 10 years. You don’t have to quit everything to save yourself. Just make one smart choice. And then another. You got this.