Antihistamine Tolerance: Why Your Allergy Meds Stop Working and What to Do
When you first take an antihistamine, a medication that blocks histamine to reduce allergy symptoms like sneezing, itching, and runny nose. Also known as H1 blockers, they’re one of the most common over-the-counter fixes for seasonal allergies. But if you’ve been using the same one for months—maybe even years—you might notice it’s not working like it used to. That’s not in your head. It’s antihistamine tolerance, and it’s more common than you think.
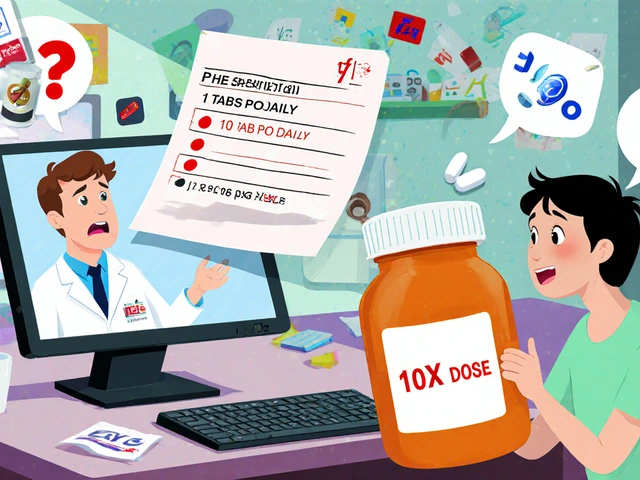
Antihistamine tolerance happens when your body gets used to the drug, and the dose that once shut down your symptoms no longer does. This isn’t addiction—it’s pharmacological adaptation. Your histamine receptors become less responsive, or your body starts breaking the drug down faster. First-gen antihistamines like diphenhydramine (Benadryl) are the worst offenders because they cross into the brain and cause drowsiness, which your nervous system quickly adapts to. But even second-gen ones like loratadine or cetirizine can lose their edge over time, especially if you take them daily. The real problem? You start doubling up, thinking more is better. That’s when side effects like dry mouth, dizziness, or even heart rhythm issues creep in.
What’s worse, tolerance doesn’t just make your meds less effective—it can make you more sensitive to allergens. Your body’s defense system, already on high alert from constant exposure, starts overreacting to smaller triggers. This creates a cycle: more symptoms → more antihistamines → more tolerance → worse reactions. And it’s not just about pills. Nasal sprays like oxymetazoline (Afrin) cause rebound congestion if used too long, which is a form of tolerance too. The good news? You can break this cycle. Switching to a different class of antihistamine, using them only when needed instead of daily, or combining them with saline rinses or steroid sprays can reset your system. Some people find that taking a short break—just a week or two—brings back the original effectiveness.
There’s also a bigger picture here. Not everyone reacts the same way. Genetics play a role—some people metabolize antihistamines faster due to liver enzymes like CYP2D6, which means they need higher doses just to feel the same effect. And if you’re taking other meds, like certain antidepressants or antibiotics, they can interfere with how antihistamines work. That’s why seeing a doctor isn’t just about refills—it’s about understanding your body’s unique response. The posts below cover exactly this: how to spot tolerance early, why non-sedating options are safer for long-term use, how workplace safety gets affected, and what alternatives actually work without the rebound effect. You’ll find real advice on managing allergies without falling into the trap of diminishing returns. No fluff. Just what you need to take back control.