Neurorehabilitation: Recovery Strategies for Brain and Nerve Injuries
When the brain or nerves get damaged—from a stroke, accident, or disease—neurorehabilitation, a targeted process to restore function after neurological injury. Also known as neurological rehabilitation, it’s not just about getting stronger. It’s about retraining the brain to find new paths for movement, speech, and control when old ones are broken. This isn’t magic. It’s science. And it works, even when recovery feels slow.
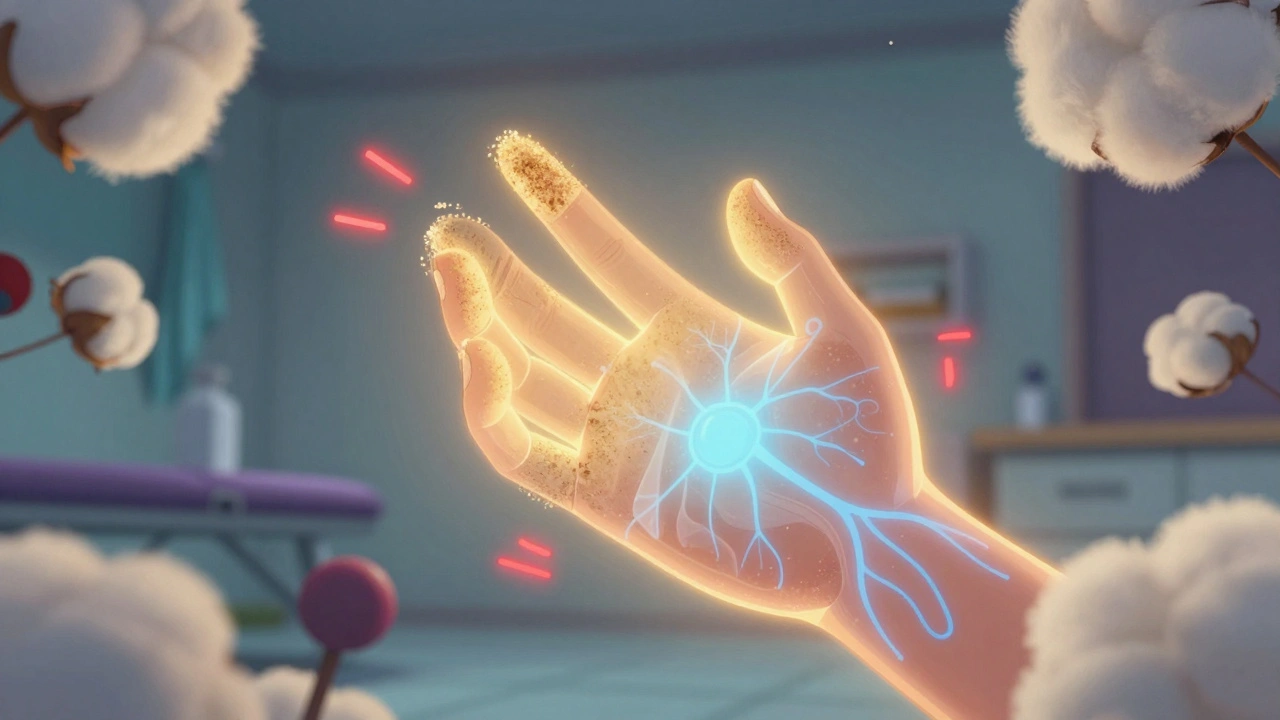
Neurorehabilitation isn’t one-size-fits-all. It’s built around the person. Someone recovering from a stroke, a disruption in blood flow to the brain causing loss of function might need help walking again. Someone with nerve damage, injury to peripheral nerves affecting sensation or muscle control from diabetes or surgery might need to relearn how to feel their fingers. And for those with brain injury, trauma or swelling that alters cognition, emotion, or movement, therapy often includes memory drills, mood support, and daily routine rebuilding. The goal? Not just to survive, but to live again.
What makes neurorehabilitation different from regular physical therapy? It’s the focus on neuroplasticity—the brain’s ability to rewire itself. Tools like robotic exoskeletons, virtual reality balance trainers, and electrical nerve stimulators are now common. But the real engine is repetition. Doing the same movement, the same task, over and over, even when it’s hard, trains the brain to adapt. Medications can help manage spasticity or pain, but they don’t rebuild function. That’s where therapy comes in. And it’s not just done in clinics. Home-based programs, telehealth check-ins, and wearable sensors are making progress more consistent and measurable.
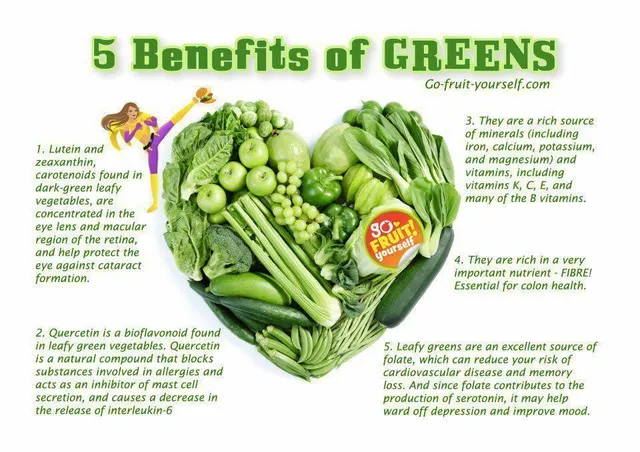
You’ll find posts here that connect directly to this journey. From managing side effects of drugs used in recovery, to using home health services for daily care, to tracking medication schedules so nothing interrupts progress. There’s advice on avoiding food-drug interactions that could slow healing, and how to spot fake meds that could hurt more than help. You’ll see how technology like FDA-approved apps and implants help patients regain independence. And you’ll learn how genetic differences can affect how someone responds to rehab drugs—why what works for one person might not work for another.
Neurorehabilitation isn’t a quick fix. It’s a daily commitment. But every small win—a step taken without help, a word spoken clearly, a hand that grips again—adds up. This collection gives you the facts, the tools, and the real-world strategies that actually move the needle. No fluff. Just what works.