Vascular Dementia: Causes, Symptoms, and How to Manage It
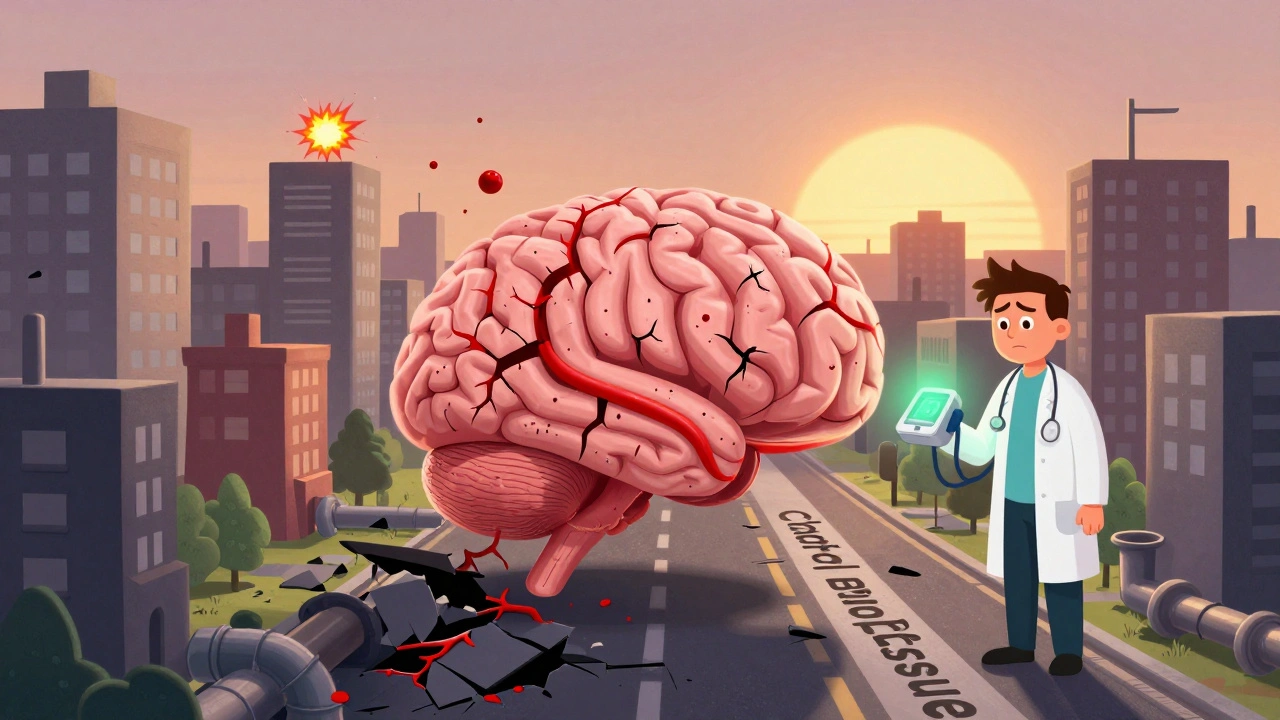
When blood flow to the brain gets blocked or reduced, it can lead to vascular dementia, a type of cognitive decline caused by damaged blood vessels in the brain. Also known as stroke-related dementia, it doesn’t happen all at once—it builds up over time from small strokes, tiny bleeds, or chronic poor circulation. Unlike Alzheimer’s, where memory loss comes first, vascular dementia often shows up as trouble with planning, slow thinking, or sudden changes in mood after a stroke.
This condition is closely tied to high blood pressure, a major risk factor that weakens blood vessel walls over time, and diabetes, which damages small vessels and reduces oxygen delivery to brain cells. You can’t reverse the damage already done, but you can stop it from getting worse. Controlling blood pressure, quitting smoking, managing cholesterol, and staying active are the most effective ways to protect your brain. Many people don’t realize that what’s good for the heart is also critical for the mind.
The symptoms can be confusing because they overlap with other conditions. One day you’re fine, the next you’re struggling to follow a conversation or forget where you put your keys. That’s not just aging—it could be vascular dementia. The key is catching it early. If you’ve had a stroke or transient ischemic attack (TIA), your risk jumps significantly. Regular check-ups and tracking changes in thinking or behavior matter more than you think.
Below, you’ll find real, practical advice from people who’ve dealt with this—how to manage medication side effects, avoid interactions that hurt cognition, use home health services to stay safe, and track what’s working. There’s no magic cure, but with the right support, you can keep your independence longer and reduce the chances of further damage.