
Ever taken a pill and felt weird afterward? Maybe your stomach churned, your head spun, or your skin broke out. You weren’t imagining it. Side effects aren’t random glitches-they’re the predictable, and sometimes unpredictable, results of how drugs interact with your body at a molecular level. The truth is, medication side effects aren’t a flaw in the system. They’re a natural consequence of how medicine works: drugs don’t just target the problem. They touch everything in their path.
How Drugs Work-And Why They Can’t Help But Cause Trouble
Think of your body like a city with thousands of buildings, each with its own function. A drug is like a key designed to unlock one specific door-the one linked to your illness. But here’s the catch: many keys don’t fit just one lock. They can slip into others, too. That’s called an off-target effect. For example, NSAIDs like ibuprofen are meant to block COX-2, an enzyme that causes pain and swelling. But they also block COX-1, which protects your stomach lining. That’s why up to 30% of regular users end up with stomach irritation or ulcers. It’s not a mistake. It’s biology. Even drugs meant for the brain don’t stay there. Haloperidol, used to treat psychosis, blocks dopamine receptors in the brain to calm hallucinations. But dopamine receptors are also in the basal ganglia, which controls movement. So, 30-50% of people on this drug develop tremors or stiffness within days. The drug didn’t fail. It just didn’t know how to pick just one target.Your Genes Decide How Your Body Handles Drugs
Not everyone reacts the same way to the same pill. Why? Because your genes control how your body breaks down medications. A group of liver enzymes called cytochrome P450 handles most drug metabolism. But people have variations in these enzymes. About 5-10% of Caucasians are “poor metabolizers” of CYP2D6. That means codeine, which needs to be converted into morphine to work, stays inactive in their bodies-or, worse, gets converted too slowly, leading to dangerous buildup. In some cases, this causes life-threatening breathing problems. Then there’s HLA-B*57:01, a gene variant that makes people extremely sensitive to abacavir, an HIV drug. Before testing, about 5-8% of carriers had severe allergic reactions. Now, doctors screen for this gene first. The result? Reactions dropped to less than 0.5%. That’s not luck. That’s precision medicine in action.When Your Immune System Turns Against the Drug
Some side effects aren’t about chemistry-they’re about your immune system going rogue. These are called hypersensitivity reactions. Type I reactions, like anaphylaxis from penicillin, happen fast-within minutes. About 1 in 10,000 people get this. It’s scary, but rare. Other reactions are slower. Type IV reactions, driven by T-cells, can take weeks to show up. Stevens-Johnson Syndrome, a deadly skin condition, is one of them. It’s most often triggered by allopurinol, sulfonamides, or seizure meds. The risk? Just 1-6 cases per million people each year. But when it happens, it’s life-threatening. Then there are pseudoallergic reactions-like vancomycin flushing. It looks like an allergy: red skin, itching, low blood pressure. But it’s not immune-driven. The drug directly triggers mast cells to dump histamine. That’s why doctors give it slowly. Speed matters.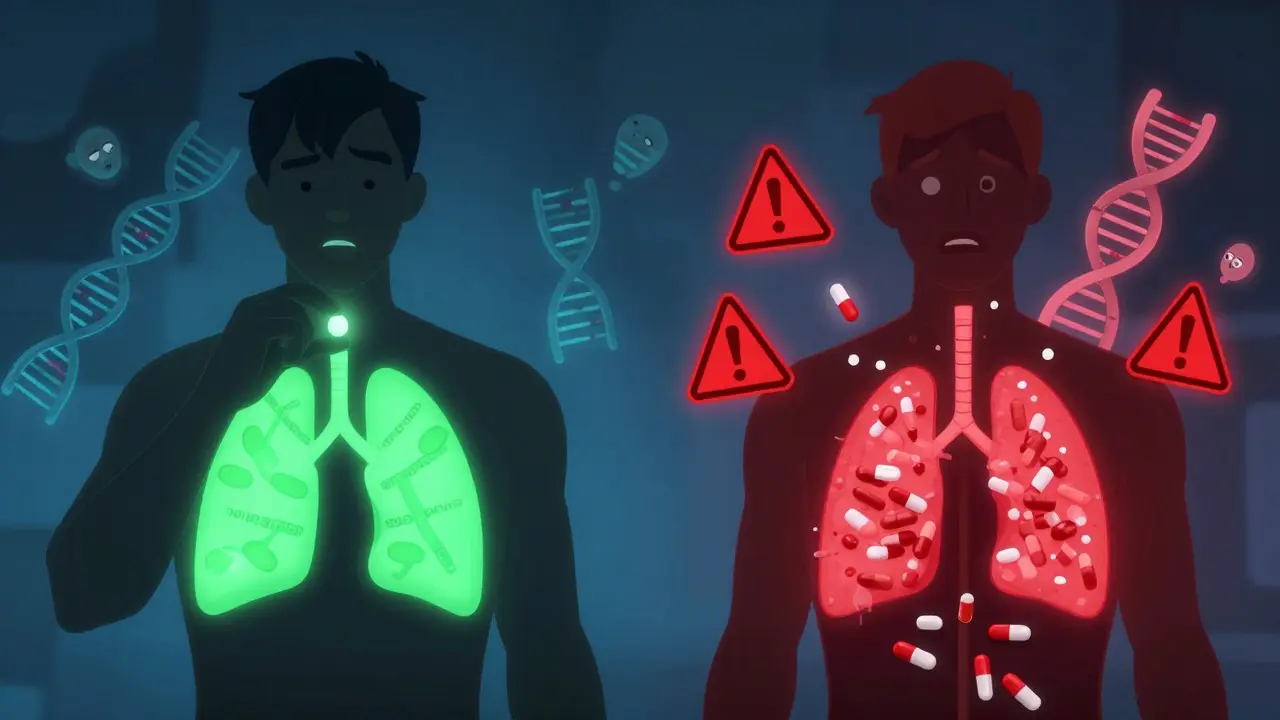
Drugs Don’t Just Float Around-They Change Your Cells
A 2021 study from Weill Cornell Medicine showed something surprising: drugs can mess with your cell membranes. Most drugs don’t just bind to proteins. They also change the physical properties of the membrane itself-its thickness, flexibility, or charge. Think of it like pouring oil into a machine. It doesn’t break the gears, but it changes how they move. That’s why some drugs affect dozens of unrelated proteins. It’s not that they’re designed to. It’s that the membrane doesn’t care which protein it touches-once it’s disturbed, everything wobbles. This explains why some drugs cause weird, scattered side effects. A drug meant for the heart might also affect the liver or nerves. Not because it’s poorly designed-but because the membrane is a shared space.Drug Interactions: When One Pill Makes Another Dangerous
Taking multiple meds is common. But each one can interfere with the others. Grapefruit juice isn’t just a healthy breakfast-it’s a drug disruptor. It blocks CYP3A4, an enzyme that breaks down many drugs. One glass can make felodipine, a blood pressure med, 260% more potent. Result? Dangerously low blood pressure. Rifampicin, an antibiotic, speeds up the breakdown of digoxin, a heart drug. That means the digoxin gets cleared too fast-and stops working. NSAIDs reduce kidney blood flow, which slows down methotrexate, a drug used for arthritis and cancer. Buildup can lead to bone marrow failure. Older adults on five or more medications have a 6-7% chance of being hospitalized because of interactions. It’s not just the pills. It’s the combo.
How Doctors Fight Side Effects Before They Start
Doctors aren’t just guessing anymore. They’re using science to prevent problems before they happen. Pharmacogenomic testing is now routine for some drugs. Before giving abacavir, they check for HLA-B*57:01. Before prescribing clopidogrel (a blood thinner), they test CYP2C19. Poor metabolizers? They switch to a different drug. No trial and error. For drugs with narrow safety margins-like digoxin or warfarin-doctors monitor blood levels. Digoxin needs to stay between 0.5 and 0.9 ng/mL. Too low? Ineffective. Too high? Toxic. Prophylactic meds help, too. If you’re on long-term NSAIDs, you’re often given a proton pump inhibitor to protect your stomach. That cuts ulcer risk by 70-80%. And dose timing matters. Starting an SSRI at a low dose reduces nausea and dizziness in 20-30% of patients. Slow and steady wins the race.The Future: Predicting Side Effects Before They Happen
The next big leap? Using AI to predict side effects before a drug even hits the market. Right now, about 30% of clinical trial failures are due to unexpected toxicity. That costs billions. New AI models analyze how a molecule might interact with thousands of proteins and membrane structures. One 2023 study in Nature Reviews Drug Discovery found AI could cut late-stage failures by 25-30%. The FDA’s Sentinel Initiative tracks real-world data from 300 million patients. It found that pioglitazone, a diabetes drug, increases heart failure risk by 1.5-2 times. That discovery came from real-life usage-not lab tests. We’re moving from reacting to side effects to preventing them before they start. It’s not magic. It’s data, genes, and smarter science.Bottom Line: Side Effects Aren’t a Bug-They’re a Feature of Biology
Medications cause side effects because the human body is complex, interconnected, and deeply individual. A drug can’t be perfectly targeted. Your genes shape how it’s processed. Your other meds change its behavior. Your cell membranes don’t care what the drug was meant for-they just respond to change. But here’s the good news: we’re getting better at predicting, preventing, and personalizing treatment. Side effects won’t disappear. But they’re becoming less random. Less dangerous. And more manageable.If you’ve ever been told, “It’s just a side effect,” remember: it’s not just luck. It’s science. And science is learning how to listen.
Are all side effects dangerous?
No. Many side effects are mild and temporary-like nausea, drowsiness, or dry mouth. These often fade as your body adjusts. But some, like severe rashes, breathing trouble, or liver damage, need immediate medical attention. The key is knowing which ones to watch for and when to call your doctor.
Can I avoid side effects by taking less of a drug?
Not always. Some side effects are dose-dependent, like dizziness from blood pressure meds. Lowering the dose helps. But others aren’t. For example, a genetic reaction to abacavir can happen at any dose. Never reduce your dose without talking to your doctor-it could make your condition worse.
Why do some people have side effects and others don’t?
It comes down to genetics, age, liver and kidney function, other medications, and even diet. Two people taking the same drug can have completely different experiences because their bodies handle it differently. That’s why personalized medicine is growing so fast.
Do natural supplements cause side effects too?
Yes. Just because something is “natural” doesn’t mean it’s safe. St. John’s wort can interfere with antidepressants, birth control, and blood thinners. Garlic and ginkgo can increase bleeding risk. Herbal products aren’t regulated like drugs, so their effects are less predictable.
How do I know if a side effect is serious?
Watch for signs like chest pain, trouble breathing, swelling of the face or throat, severe rash or blistering, yellow skin or eyes, unusual bleeding, or sudden confusion. If you’re unsure, call your doctor or go to urgent care. Better safe than sorry.
Can I report a side effect I experienced?
Yes. In Australia, you can report it to the Therapeutic Goods Administration (TGA). In the U.S., use the FDA’s MedWatch program. These reports help regulators spot new safety issues. Your experience could help protect others.
If you’re on multiple medications, keep a list of everything you take-including supplements-and review it with your doctor every six months. Simple steps like this can prevent big problems.





So let me get this straight - we’re giving people chemical keys to unlock one door, but those keys are made by people who clearly never took high school biology? The fact that we’re still surprised when drugs mess with your stomach, brain, or skin is the real tragedy here. This isn’t science. It’s trial by error with a billion-dollar price tag.
There’s a lot of truth in this breakdown. The body isn’t a machine with neatly labeled parts - it’s a living, breathing network where everything affects everything else. That’s why even the most targeted drugs have ripple effects. The real win isn’t eliminating side effects entirely - it’s learning to predict them before they happen. Pharmacogenomics is the future, and we’re only scratching the surface.
Wow. So drugs are like drunk roommates - they don’t know where they’re going, but they’re gonna knock over your shit anyway. And now we’re paying scientists to map the mess? Cool. I’ll take my herbal tea and my 1980s wisdom thanks.
OMG this is so important!! I had a crazy reaction to that one antibiotic and I didn’t know why until I read this. Like… my body just went full chaos mode. So glad we’re finally figuring this stuff out!!
Ugh. Another ‘science is magic’ article. They don’t even mention how pharma companies design drugs to maximize side effects so you keep buying more pills. The ‘off-target’ thing? That’s a feature, not a bug. Wake up.
Genetic variability explains so much. I’ve seen patients on the same dose of clopidogrel - one has a heart attack, the other feels fine. No mystery. Just biology. Testing should be standard, not optional.
Side effects? Please. You’re just not taking enough weed. Real medicine doesn’t need a 20-page warning label. If your body can’t handle a pill, maybe you need to eat less sugar and stop watching Netflix.
Man, this is the kind of stuff I wish my doctor explained before handing me a script. That membrane thing? Mind blown. It’s not just about binding proteins - it’s like the drug’s walking through your cells like it owns the place. No wonder you get weird side effects across the board. We need more of this in med school.
Wait wait wait - so grapefruit juice is like a drug saboteur?! I drink it every morning!! I’m gonna stop now!! And also, I just took 3 pills and now I feel like a zombie but I thought it was just Monday???
I’ve had Stevens-Johnson Syndrome. It wasn’t just a rash. It was like my skin was being peeled off while I was awake. I spent 47 days in the hospital. They didn’t even test me for the gene. Please - if you’re prescribed allopurinol or sulfa drugs - ask for the test. It could save your life.
Ohhhhh so that’s why I got dizzy after the statin… and why I had that weird rash… and why I couldn’t sleep… and why I cried during a commercial for dog food… IT’S ALL THE DRUGS!!!
The evolution from reactive to predictive pharmacology is one of the most significant advances in modern medicine. When we integrate genomic data, real-world evidence, and AI-driven modeling, we move beyond the one-size-fits-all paradigm. This isn’t speculation - it’s clinical reality unfolding in real time. The responsibility now lies with institutions to make these tools accessible, not just available.