CRPS Pain Relief: What Works and What Doesn't
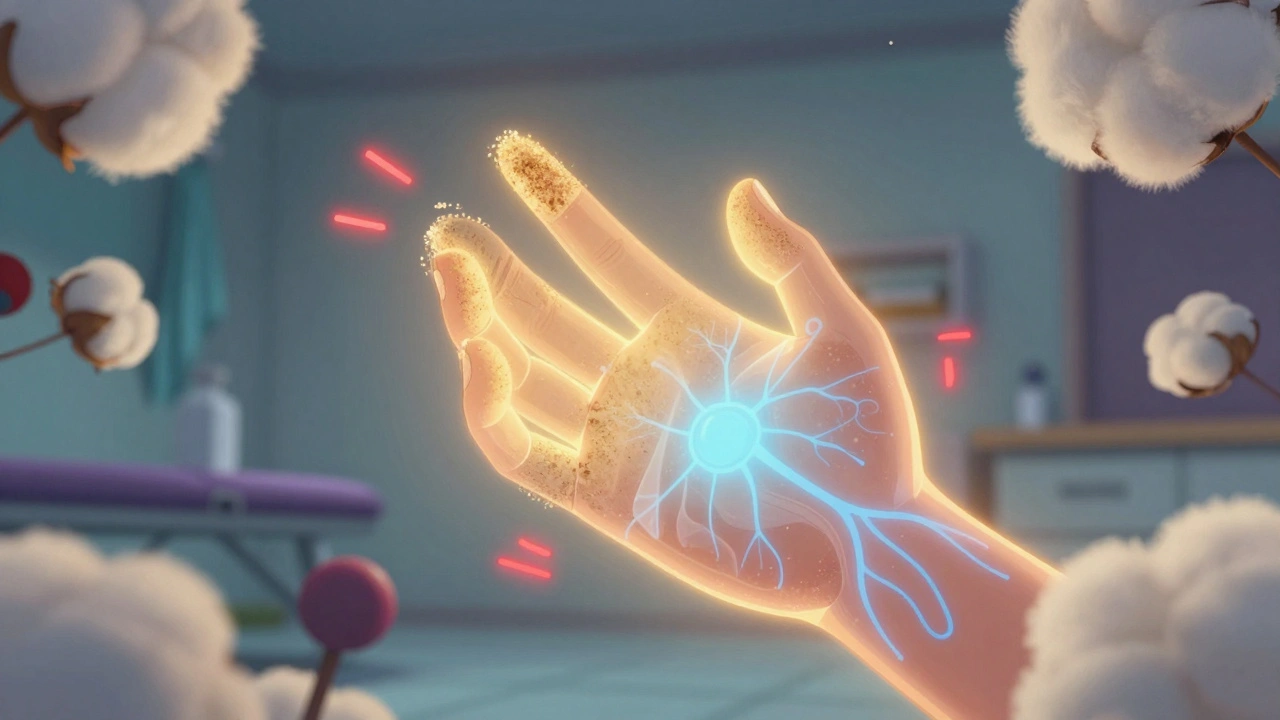
When you have complex regional pain syndrome, a chronic nerve pain condition that usually follows an injury and causes burning, swelling, and extreme sensitivity. Also known as reflex sympathetic dystrophy, it doesn’t always show up on X-rays or MRIs, but the pain is very real and often gets worse over time if not handled right. This isn’t just regular soreness or a slow-healing bruise. CRPS turns your nervous system into a faulty alarm that won’t shut off—even after the original injury healed.
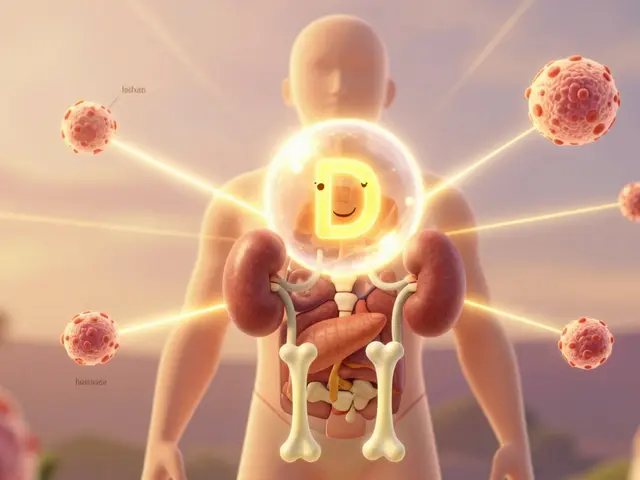
Most people with CRPS try painkillers first, but opioids and even strong NSAIDs often don’t touch the core problem. What actually helps? nerve pain treatment, specific therapies designed to calm overactive nerves, not just mask pain like physical therapy with graded motor imagery, mirror therapy, or low-dose ketamine infusions. These aren’t magic cures, but they’ve helped people regain movement and reduce pain intensity in clinical settings. Then there’s neuropathic pain, the broader category CRPS falls under, caused by damaged or misfiring nerves—and treatments that work for diabetic neuropathy or post-shingles pain often overlap with CRPS relief strategies.
What you won’t find in most guides is how often CRPS gets misdiagnosed as arthritis, tendonitis, or even psychological pain. That’s why tracking your symptoms—when they flare, what triggers them, what helps—is so critical. Some people respond to spinal cord stimulators; others find relief with gabapentin or topical lidocaine patches. But no single fix works for everyone. The key is combining approaches: movement, nerve modulation, and avoiding things that make it worse, like cold exposure or tight clothing. The posts below show real-world experiences and medical insights on what’s been tried, what failed, and what actually moved the needle for people living with this condition. You’ll see what works in practice, not just theory.