
For millions of people with obstructive sleep apnea, the CPAP machine is a nightmare - not because it doesn’t work, but because it’s impossible to live with. The mask digs into your face. The hose tangles in your sheets. The air pressure feels like a blow-dryer blasting your nose all night. And after weeks of frustration, most people give up. That’s where upper airway stimulation comes in - a hidden breakthrough for those who’ve tried everything else.
What Is Upper Airway Stimulation?
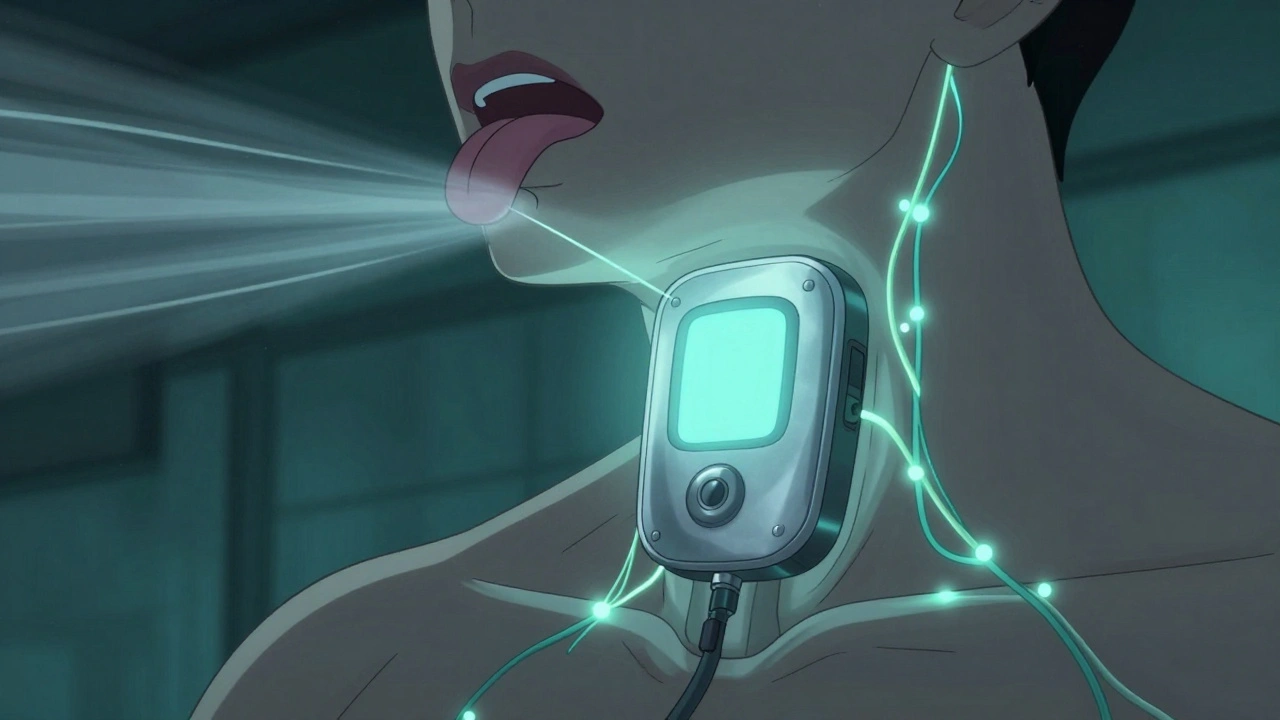
Upper airway stimulation (UAS) is a surgically implanted device that wakes up your tongue during sleep to keep your airway open. It’s not a mask. It’s not a machine you wear. It’s a small, quiet implant inside your body that senses when you breathe in and gently moves your tongue forward so it doesn’t block your throat. The most common system is called Inspire, approved by the FDA in 2014 and now used by over 200,000 people worldwide.The device doesn’t zap your throat. It doesn’t vibrate. It doesn’t hurt. It works like a pacemaker for your airway. When you inhale, a sensor triggers a mild pulse to the nerve that controls your tongue. Your tongue moves slightly forward - just enough to stop the collapse that causes apnea. Then it shuts off when you exhale. You don’t feel it. Your partner doesn’t hear it. And you sleep like you haven’t in years.
Who Is It For?
This isn’t for everyone. You need to meet specific criteria to qualify. First, you must have tried CPAP and failed. Not just struggled - actually quit. Studies show 29% to 46% of people abandon CPAP because it’s uncomfortable. If you’re one of them, UAS might be your next step.You also need to have moderate to severe sleep apnea - an AHI (apnea-hypopnea index) between 15 and 100 events per hour. If your AHI is below 15, you’re probably better off with an oral appliance. Above 100? That’s rare, but newer guidelines now include those cases too.
Your BMI should be under 35. If you’re significantly overweight, the device may not work as well. You also need to have a specific type of airway collapse - usually a blockage in the back of the tongue, not the soft palate. That’s checked with a special sleep endoscopy test. And you can’t have too many central apneas (where your brain doesn’t tell your body to breathe). That’s a different problem.
Age matters too. You must be at least 22 years old. It’s not approved for teens or older adults with complex health issues. This isn’t a quick fix. It’s a targeted solution for a very specific group.
How Does the Surgery Work?
The procedure takes about two to three hours and is done as an outpatient. You’re under general anesthesia. Three small incisions are made: one near your collarbone for the battery, one in your neck for the nerve wire, and another lower in your neck for the breathing sensor. The battery is about the size of a pacemaker. The wires are thinner than spaghetti.Unlike older throat surgeries - like removing tonsils or cutting the soft palate - this doesn’t cut or remove any tissue. It’s reversible. If you change your mind later, the device can be taken out. Recovery is quick. Most people are back to light activity in five to seven days. No hospital stay. No breathing tubes. No long healing time.
But you don’t turn it on right away. You wait about a month for the swelling to go down. Then you go back to the clinic. Your doctor connects the device to a programmer, tests the settings, and shows you how to use the remote. It’s like turning on a TV. You press a button before bed. It turns on automatically. You wake up, press it again, and it shuts off.
How Effective Is It?
The data is strong. In the STAR trial - the largest study ever done on UAS - patients saw their AHI drop from an average of 29.3 to just 9.0 in one year. That’s a 68% reduction. Two out of three patients cut their apnea events by half or more. And 86% of users say it’s better than CPAP.Real-world results match the clinical numbers. A study from the Cleveland Clinic found that 85% of bed partners reported no snoring - or just soft snoring - four years after implant. One Reddit user wrote: “My wife says I’ve stopped snoring completely after two years. I feel more rested than I have in decades.”
Daytime symptoms improve too. People report less fatigue, better focus, and fewer headaches. Blood pressure often drops. Mood lifts. Relationships improve. One patient said, “I didn’t realize how much I was snoring until my wife said she could finally sleep next to me again.”
What Are the Risks?
It’s not risk-free, but serious problems are rare. Less than 0.5% of patients have major complications. The most common issue is temporary tongue weakness - about 5% of people feel a slight numbness or tingling, and it usually fades within a few months. Minor infections at the incision sites happen in about 2% of cases. The device can sometimes shift slightly, requiring a small adjustment.Some people forget to turn it on. It’s not automatic. You have to remember to press the remote every night. That’s the biggest behavioral hurdle. If you skip it, you’ll still have apnea. But once it becomes part of your routine - like brushing your teeth - it’s easy.
There’s also the cost. The total price ranges from $35,000 to $40,000. That sounds high. But when you factor in the cost of CPAP machines, masks, repairs, follow-up visits, and lost productivity from poor sleep, UAS can pay for itself in three to five years. And insurance covers it for most people now - 95% of Medicare and 85% of private plans include UAS in their benefits.

How Does It Compare to Other Treatments?
Let’s break it down:- CPAP: Works for 70% of people - if they use it. But 3 out of 10 quit within a year. It’s non-invasive, but the discomfort is real.
- Oral Appliances: Custom mouthpieces that push your jaw forward. Good for mild to moderate cases. Less effective for severe apnea. Can cause jaw pain or tooth movement.
- Traditional Surgery: Procedures like UPPP remove tissue from the throat. Painful. Long recovery. Often doesn’t work long-term. Not reversible.
- Upper Airway Stimulation: No masks. No removal of tissue. Reversible. Works for severe cases. High satisfaction. Requires surgery, but it’s low-risk and outpatient.
UAS isn’t better than CPAP for everyone. But for those who can’t tolerate CPAP, it’s the best option available - better than surgery, more reliable than mouthpieces, and far more effective than doing nothing.
What’s Next for This Therapy?
The technology is still evolving. In 2023, the FDA expanded eligibility to include patients with BMI up to 40 and AHI up to 100. That opened the door for thousands more. Researchers are now using AI to predict who will respond best - analyzing airway scans before surgery to avoid implanting in people who won’t benefit.Next-gen devices are getting smaller. One prototype is half the size of the current Inspire unit. Battery life is improving too. Future versions may even auto-detect breathing without needing a separate sensor.
As more doctors learn how to use it, and as insurance coverage expands, UAS is moving from a last-resort option to a mainstream treatment. The global market for sleep apnea devices is growing at 14% per year - and UAS is leading the charge.
What Should You Do If You’re Considering It?
Start with a sleep study if you haven’t had one in the last two years. Then talk to a sleep specialist who’s trained in UAS. They’ll refer you for a drug-induced sleep endoscopy - a quick, outpatient test that shows exactly where your airway collapses.If you qualify, your insurance will likely cover the evaluation. The implant center will handle pre-authorization. Most patients get approval within a few weeks. Then it’s surgery, recovery, and activation.
Don’t wait until you’re exhausted all day. Don’t wait until your partner sleeps on the couch. Don’t wait until your blood pressure keeps climbing. If CPAP isn’t working for you, upper airway stimulation isn’t just an option - it’s your next chance at real sleep.
Is upper airway stimulation the same as a pacemaker?
It works similarly - both are implanted devices that send electrical pulses to nerves. But while a pacemaker regulates heart rhythm, upper airway stimulation targets the hypoglossal nerve to move the tongue during breathing. The hardware looks similar, but the function is completely different.
Can I have an MRI with the implant?
Yes, but only under specific conditions. The Inspire device is MRI-conditional, meaning you can have an MRI of your head or neck if the machine is set to certain settings and the device is turned off before the scan. Full-body MRIs are not allowed. Always inform your radiology team you have an implant before any scan.
Does the device ever need to be replaced?
The battery lasts about 8 to 11 years, depending on usage. When it runs low, you’ll get a warning from your remote. Replacing the battery requires a minor surgery - same incisions, same recovery. The nerve wires stay in place. It’s not a full replacement, just a battery swap.
Will I feel the stimulation all the time?
No. The stimulation only happens during inhalation. Most people don’t feel anything after the first few weeks. A small number feel a slight tingling or pulling sensation, especially at higher settings. Your doctor can adjust the intensity during follow-up visits to make it comfortable.
Can I travel with the device?
Absolutely. The remote is small and fits in your pocket. Airport security scanners won’t trigger alarms, but you may be asked to show your patient ID card. Carry it with you - it explains the device and helps avoid delays. You can fly, drive, or go on vacation without restrictions.
How long does it take to see results?
Most patients notice better sleep within the first week after activation. But it takes 2 to 4 weeks for the body to fully adjust to the stimulation. The full benefits - less daytime sleepiness, improved mood, lower blood pressure - usually show up after 3 to 6 months. Patience is key. This isn’t an instant fix, but the results last.
Upper airway stimulation isn’t magic. But for the right person - someone who’s tried CPAP, knows how bad their sleep apnea is, and is ready to take control - it’s life-changing. No mask. No noise. No more nights spent staring at the ceiling. Just quiet, deep, restorative sleep - the kind you forgot even existed.







UAS is a game-changer for severe OSA patients who can’t tolerate CPAP - the hypoglossal nerve stimulation is elegantly targeted, and the fact that it’s reversible makes it way less intimidating than ablative surgeries. The STAR trial data is solid, and real-world adherence is way higher than CPAP. Still, the screening process is brutal - not everyone’s anatomy lends itself to this, and that endoscopy is non-negotiable.
If you’re reading this and you’re tired of waking up like you got hit by a truck every morning - stop waiting. Stop blaming yourself. This isn’t a luxury, it’s a medical necessity. I’ve seen patients go from barely functional to running 5Ks after this implant. Your sleep is worth fighting for. Don’t let fear of surgery keep you exhausted.
we are all just breathing ghosts in a machine of our own making.
Hey, just curious - has anyone here had the battery replacement? I heard it’s way less invasive than the original surgery, but I’m wondering how the recovery compares. Also, does the remote ever get lost? My wife says I’d forget to turn it on if it wasn’t attached to my keychain.
It’s fascinating how medicine has evolved from brute-force interventions like UPPP to something so… elegant. A pacemaker for your tongue? Who would’ve thought? This is the kind of innovation that makes you proud to be alive in this era - not some half-baked, overpriced gadget, but a precision neurostimulation system that respects human biology. The fact that it’s FDA-approved and covered by 95% of Medicare plans? That’s not luck. That’s progress. And yet, so many still cling to CPAP like it’s a moral virtue. Sad.
Just got mine activated 3 weeks ago. First night? Slept through the whole thing. No mask, no noise, no waking up gasping. My wife cried. I didn’t even know I was snoring that loud. The tingling? Felt like a tiny buzz at first, now I forget it’s there. Only thing I miss? The CPAP machine’s white noise. Weird, right? Now I just press the remote like a TV. Life-changing. If you’re on the fence - get the endoscopy. You’ll know if you’re a candidate.
Wait - so you’re telling me I can pay $40K, get surgery, and still have to REMEMBER to turn it on? Like a damn alarm clock? And if I forget? Back to apnea? That’s not a solution - that’s a babysitter with electrodes. And don’t get me started on the MRI restrictions. What if I need a full-body scan for cancer? Do I just… die? This feels like a luxury toy for people who can afford to be ‘sleep-optimizers’ while the rest of us are stuck with $50 masks and guilt trips.
Thank you for sharing this comprehensive overview. The clinical outcomes are compelling and the procedural safety profile is remarkably favorable. For patients who have exhausted non-invasive modalities and meet anatomical criteria, this intervention represents a paradigm shift in therapeutic efficacy. The long-term adherence data and quality-of-life improvements are statistically and clinically significant. I encourage all sleep specialists to consider referral pathways for qualified candidates.
Okay but what if I just sleep on my side? Or wear a neck brace? Or hang upside down? I’ve been doing all three and my snoring sounds like a tuba in a wind tunnel. Maybe this device is just corporate hype wrapped in a fancy FDA stamp. Also, who designed the remote? It looks like a key fob from a 2007 Prius.