Most people think of vitamin D as the bone vitamin. You take it to prevent rickets or osteoporosis. But here’s the truth: vitamin D is a hormone. And like every hormone, it talks to your endocrine system - the network of glands that control everything from blood sugar to blood pressure to immune responses. If your vitamin D levels are off, it doesn’t just affect your bones. It can throw off your entire hormonal balance.
How Vitamin D Works as a Hormone
Vitamin D isn’t just a nutrient you get from food or sun. It’s a precursor to a hormone called calcitriol. Your skin makes vitamin D3 when UVB rays hit it. Then your liver turns it into 25-hydroxyvitamin D - the form doctors test. Finally, your kidneys convert that into the active hormone: 1,25-dihydroxyvitamin D. That’s the real player.
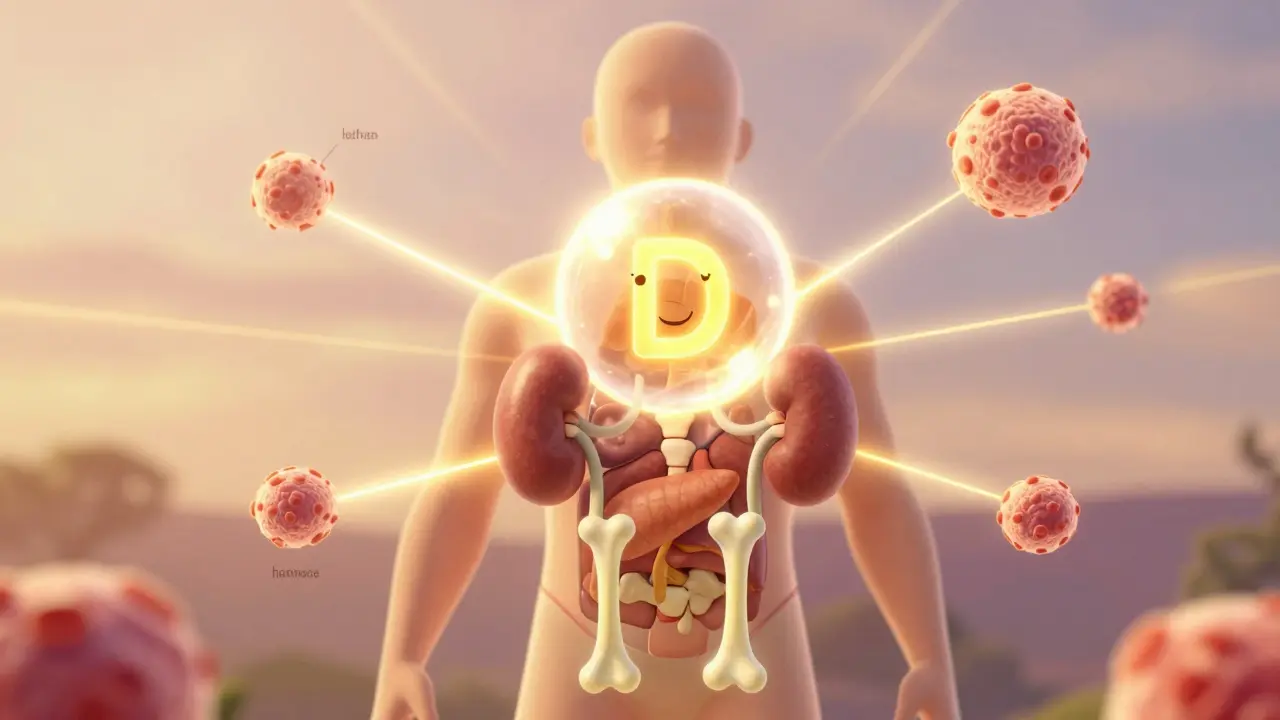
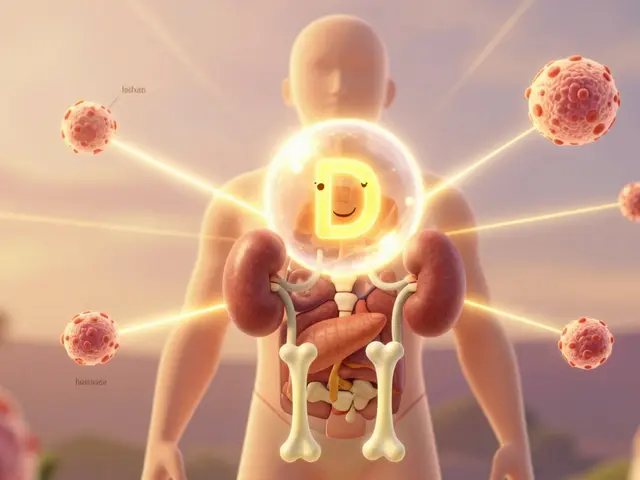
This hormone doesn’t just act in one place. It binds to receptors in almost every tissue: your intestines, kidneys, bones, immune cells, pancreas, even your blood vessels. That’s why low vitamin D is linked to more than just weak bones. It’s tied to insulin resistance, high blood pressure, autoimmune conditions, and even mood changes.
The Endocrine Society says a level below 20 ng/mL is deficient. Between 21 and 29 ng/mL is insufficient. You want at least 30 ng/mL. But here’s the twist: some people with 25 ng/mL feel fine. Others with 40 ng/mL still have symptoms. Why? Because what matters isn’t just what’s in your blood - it’s what’s happening in your tissues.
The Two Ways Vitamin D Works: Endocrine vs. Autocrine
There’s the classic endocrine pathway. Your kidneys make calcitriol based on calcium and phosphate levels. It tells your gut to absorb more calcium, your bones to release it if needed, and your kidneys to hold onto it. This keeps your blood calcium steady - between 8.5 and 10.5 mg/dL. That’s non-negotiable. Too low, and your muscles twitch. Too high, and your kidneys get damaged.
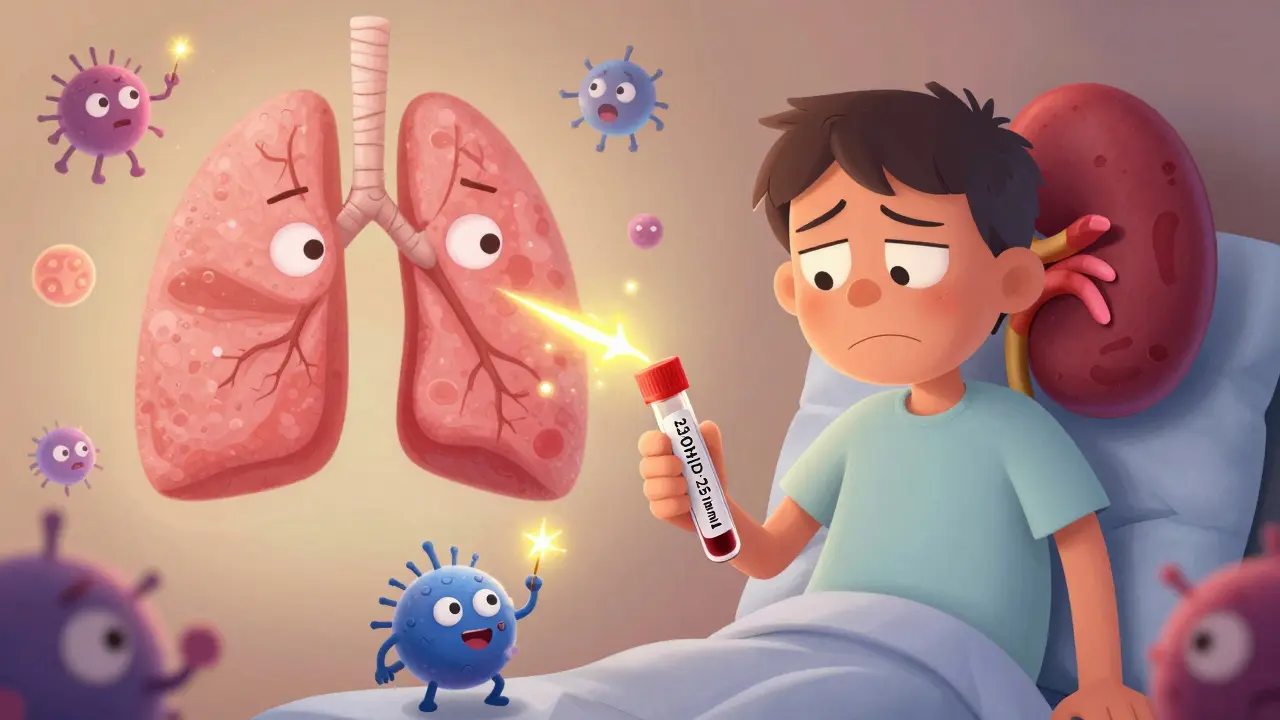
But there’s another system: the autocrine pathway. This is where your immune cells, pancreas, or skin make their own calcitriol locally - right where it’s needed. And here’s the kicker: this doesn’t depend on your blood levels at all. A macrophage in your lung can crank out calcitriol during an infection, even if your serum 25(OH)D is 18 ng/mL. That’s why some people with low blood levels still have strong immune responses - and why others with high levels still get sick.
This is the core problem with testing. A blood test tells you about your kidney’s output. It doesn’t tell you if your immune cells have enough. That’s why studies on vitamin D and cancer or heart disease are so messy. You’re measuring the wrong thing.
Who Needs Testing - And Who Doesn’t
Most healthy adults don’t need a vitamin D test. The U.S. Preventive Services Task Force says screening asymptomatic people doesn’t help. But certain groups do.
- People with osteoporosis or fractures - up to 50% are deficient
- Those with chronic kidney disease - 60-70% have low levels
- People with celiac, Crohn’s, or gastric bypass surgery - up to 90% are deficient
- Obese individuals - fat traps vitamin D, so you need 2-3 times more
- Older adults over 70 - skin makes less, and kidneys convert less
For everyone else? Skip the test. Unless you have symptoms - muscle weakness, chronic fatigue, frequent infections - there’s no proven benefit to knowing your number.
Supplementation: What Works, What Doesn’t
The VITAL trial followed 25,871 people for over five years. Half took 2,000 IU of vitamin D3 daily. The other half took a placebo. At the end, there was no difference in cancer rates, heart attacks, or strokes. Same results in other big trials. So why do people swear it helped them?
Because for some, it did. If your level was 12 ng/mL and you had muscle pain or constant tiredness, raising it to 40 ng/mL can feel like a miracle. That’s real. But if your level was already 30 ng/mL, adding more won’t help. It’s like giving insulin to someone who isn’t diabetic.
The Endocrine Society recommends:
- 600-800 IU/day for adults under 70
- 800-2,000 IU/day for adults over 70
- Up to 4,000 IU/day is safe for most - but don’t go higher without monitoring
For obese people? Start at 3,000-4,000 IU/day. For those with malabsorption? You might need 50,000 IU weekly for a few months, then switch to maintenance. And always retest after 3 months. Vitamin D doesn’t jump up overnight. It takes time.
Why Some People Don’t Respond
Not everyone absorbs or uses vitamin D the same way. Your genes matter. Some people have a variant in the CYP2R1 gene - the one that turns vitamin D into its first active form. Their bodies just don’t convert it well. Others have a DBP gene variant that binds vitamin D too tightly. That means even if their blood level looks fine, their cells can’t access it.
That’s why two people taking the same dose can end up with wildly different levels. One hits 50 ng/mL. The other stays at 22. It’s not about compliance. It’s biology.
And then there’s the issue of form. Vitamin D3 (cholecalciferol) from animal sources is more effective than D2 (ergocalciferol) from plants. Stick with D3. And take it with a meal that has fat. It’s fat-soluble. Without fat, you’re wasting it.
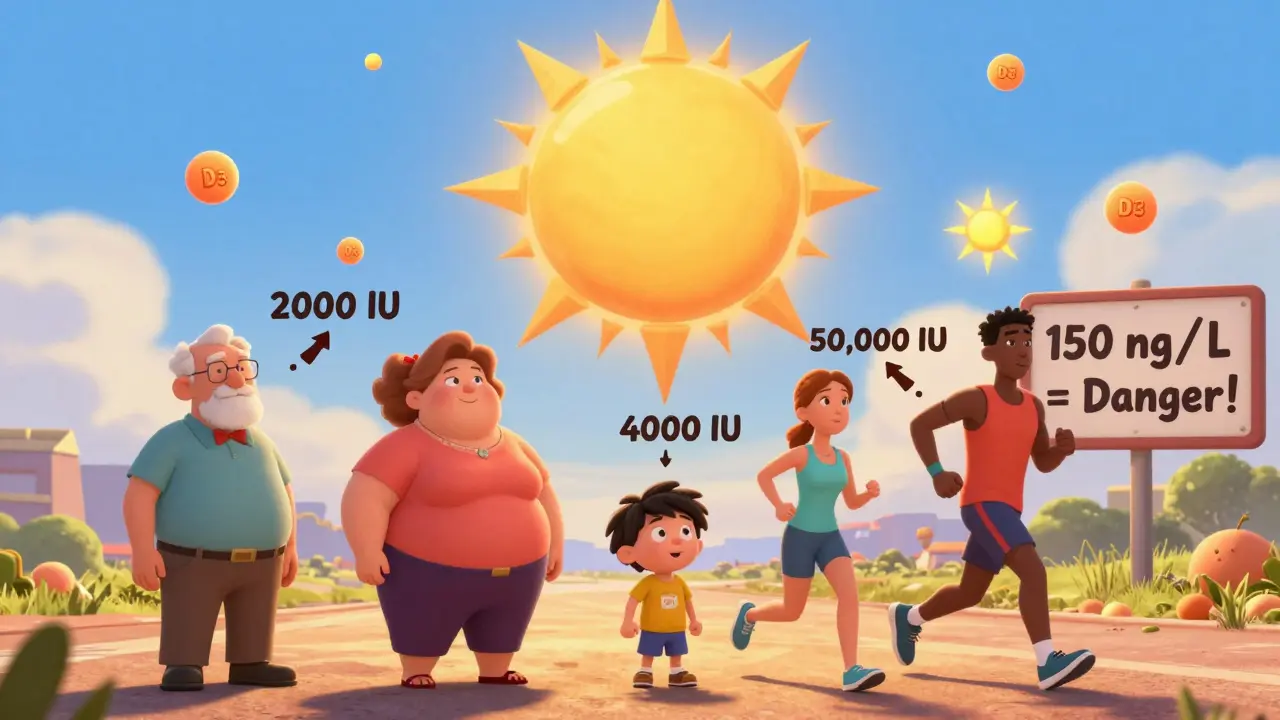
The Risks of Too Much
It’s possible to get too much. Toxicity is rare, but it happens. The threshold? A blood level over 150 ng/mL. That usually means taking 10,000 IU or more daily for months. Symptoms? Nausea, vomiting, weakness, kidney stones, even heart rhythm problems.
But here’s the catch: toxicity isn’t just about dose. People with sarcoidosis or certain lymphomas can make excess calcitriol on their own. They can become toxic even with normal supplementation. That’s why you never give high-dose vitamin D without checking calcium levels first.
The Future: Beyond the Blood Test
Researchers are tired of guessing. The NIH is funding a $12.5 million project to measure vitamin D activity directly in immune cells. They’re looking at which genes turn on when vitamin D binds to its receptor - a true biomarker of tissue-level activity.
Meanwhile, drug companies are designing smarter vitamin D analogs. One called VDRM-110 targets only the pancreas to help insulin production - without raising calcium. Another, eldecalcitol, is already approved in Japan for osteoporosis and reduces fractures better than standard vitamin D.
The message? We’re moving past the one-size-fits-all approach. In five years, we may test not just your 25(OH)D level - but how your cells are using it.
What You Should Do Right Now
If you’re healthy, active, and get some sun, you probably don’t need supplements. Eat fatty fish, eggs, fortified milk. Walk outside 15 minutes a day in the morning sun. That’s enough for most.
If you’re in a high-risk group - or you’re constantly tired, achy, or get sick often - get tested. If your level is below 30 ng/mL, start with 2,000 IU of D3 daily. Re-test in 3 months. Adjust if needed. Don’t go above 4,000 IU without medical supervision.
And forget the hype. Vitamin D won’t cure your diabetes, prevent your cancer, or fix your depression. But if you’re deficient, fixing it can restore your energy, reduce your fracture risk, and help your immune system work right. That’s not magic. That’s physiology.
Don’t take more than you need. Don’t test without reason. And don’t believe everything you read online. The science is complicated. But the goal is simple: keep your levels in the range your body was designed for - not the range a supplement company wants you to be in.






Okay but let’s be real-how many of us are even getting enough sun anymore? I work from home, wear sunscreen like it’s my job, and my vitamin D is still in the toilet… Meanwhile, my cat gets more sunlight than I do, and she’s fine. 🐱
I took 5000 IU for 6 months because my doctor said ‘maybe’ and now I feel like a new person. No more 3pm crashes, no more brain fog. I’m not saying it’s magic-but it’s definitely not placebo. 🌞💖
Interesting breakdown. I’ve always thought of it as just ‘bone stuff’ too. Didn’t realize it was basically a master hormone. Makes me wonder how many other ‘simple’ supplements are actually way more complex than we think.
Of course the Endocrine Society says 30 ng/mL is ideal. They’re funded by pharma. The real truth? You don’t need supplements if you eat real food and get outside. This whole vitamin D industry is a scam to sell pills.
In India, we don’t even have access to proper testing. My cousin took 10,000 IU daily because she saw it on Instagram and now her calcium is sky-high. Doctors just shrug. This is why we need regulation, not more supplements.
Love how you broke this down. I used to think D3 was just for bones too-until I started feeling better after a year of low-dose D3 with my dinner. Fat matters. Timing matters. And yes, I retested. Went from 22 to 44. No side effects. Just… energy. 🙌
Stop taking random doses! If you’re tired, get tested-not because you read a Reddit post, but because your body’s telling you something. I was at 14 ng/mL and thought I was just ‘lazy.’ Turns out, I was vitamin D deficient. Changed my life. Don’t be like me-figure it out before you burn out.
It’s funny how people treat vitamin D like a cure-all. It’s not. It’s a hormone. You wouldn’t inject insulin if you weren’t diabetic. Why treat vitamin D like it’s a magic bullet? The science is nuanced. Most people don’t need it. The rest need a doctor-not a YouTube influencer.
My uncle in rural India takes sun every morning before work. No supplements. No tests. He’s 78 and walks 5 miles daily. Maybe the answer isn’t pills. Maybe it’s just being outside. Simple. Free. Real.
They don’t want you to know the truth. The FDA, WHO, Big Pharma-they all profit from you taking pills. Sunlight is free. Vitamin D from sun is regulated by your body. Pills? That’s control. And they’re lying to you about the real risks. Watch out.
So you’re telling me the same dose gives one person 50 and another 22? And we’re supposed to trust blood tests? That’s like measuring a car’s speed by how much gas is in the tank. Brilliant. I’m just gonna sit in the sun and laugh.
Stop taking supplements. You don’t need them. Sunlight is enough. End of story.
Okay, but what about the autocrine thing? That’s wild. So my immune system could be making its own calcitriol even if my blood level is low? That explains why I get sick less than my sister even though her labs are ‘perfect.’
While the autocrine pathway is indeed a biologically plausible mechanism, the clinical relevance remains empirically unvalidated in large-scale, randomized controlled trials. The current evidence base does not support the notion that tissue-level vitamin D activity, as inferred from serum concentrations, confers a statistically significant health benefit beyond established endocrine functions. Therefore, population-wide supplementation remains unsupported by robust epidemiological data.